[The cellular microenvironment: a cornerstone of advances in regenerative corneal medicine?].
Regenerative medicine aims to replace or regenerate cells, tissues or organs lost due to a variety of causes. Over the last decade, this field has undergone significant transformations, with the development of modern therapies and the dissemination of new materials. Significant progress has been made in the case of the cornea, with progress in the development of stem cell therapy, 3D printing, bioengineering of the cornea, gene therapy and exosome treatments. They are all changing the way corneal diseases are treated and offering hope to millions of people with visual impairments.
When we talk about corneal regeneration, we often represent the replacement of damaged cells, but today in the European Union, stem cell and amniotic membrane graft transplants are available for the treatment of corneal diseases. In addition, a number of studies and clinical trials are underway to develop new methods and materials, highlighting the need in this area. The combination of cell therapy and biomaterials and the clarification of the importance of the microenvironment have opened the way to integrative solutions that go far beyond traditional treatments such as corneal transplants.
At the heart of this breakthrough, the cellular microenvironment is a component of vital importance. It plays an active and essential role in the success of regenerative therapies. It is believed that the basis for new corneal regeneration solutions may be the interaction between cells, biomaterials and the environment surrounding them, which is what current research is focusing on. [1]
The cornea, a tissue organized in several different layers
The cornea is organized in 5 layers with different characteristics and functions, and the interaction of all is necessary for its visualization: epithelium, Bowman's membrane, stroma, Descemet's membrane and endothelium (Figure 1).
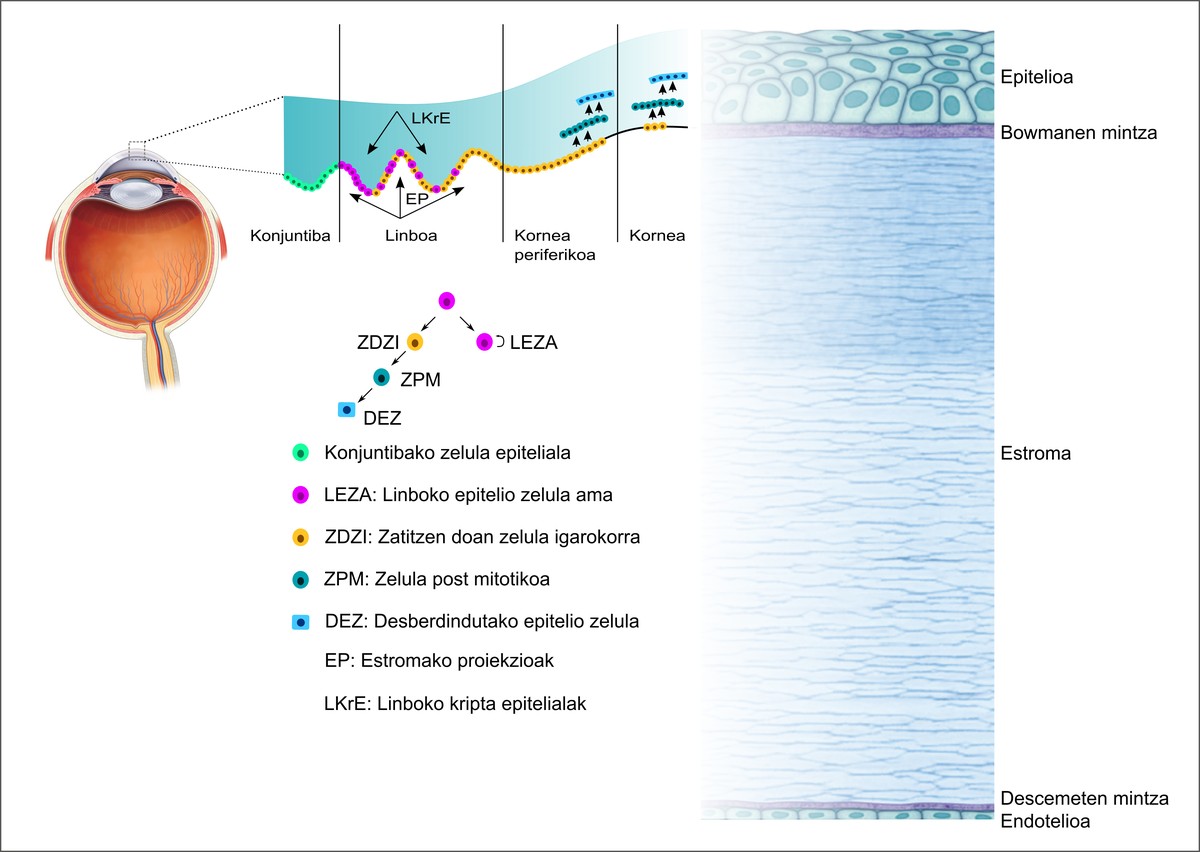
The epithelium is the outer layer that protects the tissue from external threats. At the base of the epithelium are limbal epithelial stem cells (LEZA). These cells migrate from the base to the upper layers as the surface cells become desquamated to replace the cells in the upper layers. The Bowman's membrane is located in the lower part of the epithelium and physically separates the epithelium from the underlying stroma. It is composed of a randomly organized network of collagen fibers and is the first cell-free layer of the cornea. The stroma is the layer that makes up 90% of the total cornea, and the precise organization of its extracellular matrix and keratocytes provides structural integrity and transparency to the cornea. The second acellular layer of the cornea, the Descemet membrane, is the basement membrane of the endothelium and is involved in maintaining the homeostasis, structure and transparency of the cornea. Finally, there is the endothelium, composed of cells organized in a single layer. This regulates the hydration of the tissue by pumping excess fluid out of the stroma and maintaining the clarity and function of the cornea.
If one of the aforementioned layers is damaged, its function may be lost and the vision may be compromised. Thus, regenerative therapies aim to repair or replace damaged cells in these layers while addressing problems related to their microenvironment.
The microenvironment of cells as a key to destiny
The microenvironment of cells is the área that accounts for all of the physical elements and secreted signals that surround a cell. These elements influence the behavior of the cells and the environment they produce is necessary for the survival of the cells. In the case of stem cells, they are known to be present in certain tissue niches, necessary for their maintenance to maintain the conditions there. [2] In the cornea, the sclerocorneal limbus stem cell niche clearly shows the potential effect of the microenvironment on cell function. The limbus niche provides a highly regulated, protective, and specialized microenvironment for limbus epithelial stem cells (LEZA), providing biochemical signals, structural support, and physical stimuli to maintain the potential for regeneration.
By targeting the extracellular matrix of the niche, such as the component laminins and collagens, they provide support for the regulation and retention of stem cell activity. Growth factors such as VEGF and TGF-B ensure that stem cells remain undifferentiated and are ready to respond to injury. Mechanical forces, such as flickering or stiffness of the surrounding substrate, also help to regulate stem cells.
Thus, if the microenvironment changes due to inflammation or disease or age, it is unable to sustain healthy regeneration. Thus, it is clear that effective corneal therapies must not only replace cells, but also restore or regenerate the microenvironment. [1,3]
Corneal regeneration solutions that take into account the microenvironment: Cellular therapies, biomaterials and exosomes
Regenerative medicine has made great strides in cell therapies for the cornea, and it is essential not only to replace cells, but also to maintain and optimize the microenvironment. Limbal stem cell transplantation allows the restoration of the corneal epithelium, and induced pluripotent stem cells allow tissue regeneration without the need for donor stem cells. In addition, endothelial cell therapy has led to the avoidance of whole transplants by restoring corneal endothelium with injections of cells. The cellular microenvironment plays a key role in the efficacy of these therapies, as added biomaterials, supports, or biochemical signals facilitate cell integration and survival. Exosomes derived from stem cells offer a less invasive alternative as they attempt to modulate tissue regeneration without the use of tissue grafts or cell injections. Thanks to these advances, cell therapies are transforming the treatment of corneal diseases by improving ocular tissue regeneration and reducing dependence on traditional transplants (Figure 2).
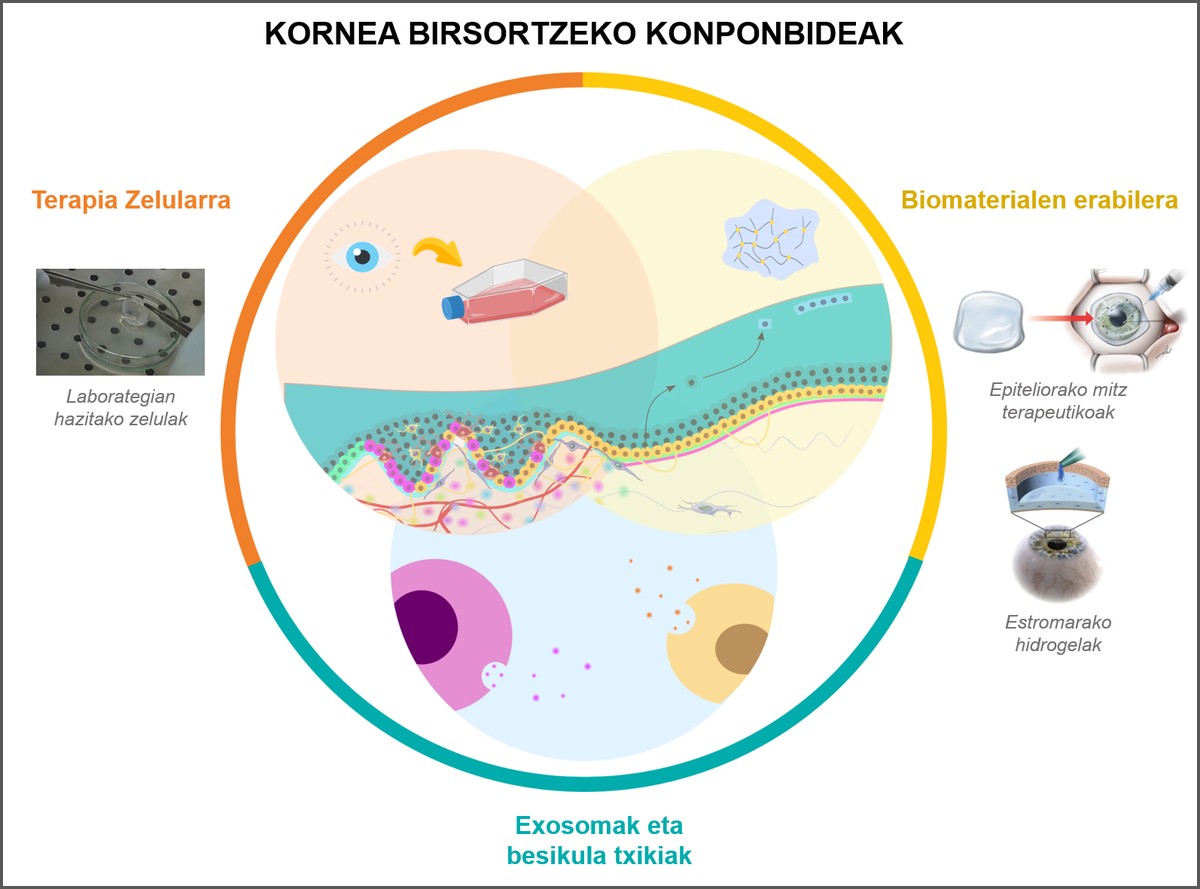
Cell therapy opens new avenues for the treatment of corneal diseases and defects
For the epithelium, LEZA transplantation is a transformative solution for people with a deficiency of lymphoid stem cells. Culturing these stem cells in the laboratory and transplanting them into the eye renews the corneal epithelial surface and prevents inflammation and scarring. In the stroma, keratocyte transplantation has the potential to restore scars and restore the structural integrity of the cornea. Finally, in the case of endothelium, injection of seeded endothelial cells into the anterior chamber of the eye has shown to restore the essential pumping function that maintains hydration and clarity. Thus, it is evident that specific treatments for the corneal layers are very effective when combined with strategies that take into account the surrounding environment.
Biomaterials expanding the catalogue of regenerative medicine
In addition to cell therapies, biomaterials are the cornerstone of today’s regenerative medicine and act as supports or transporters that help transplanted cells survive, integrate and function. They may be natural, synthetic, or a combination of both, and are designed to replicate the unique properties of the cornea, such as transparency, mechanical strength, and biological compatibility.
Human amniotic membrane or fibrin sheet or adhesives are commonly used as a support medium for these cells in LEZA transplantation. These biomaterials not only promote cell adhesion and growth, but also contribute to the reduction and healing of inflammation through intervention in the microenvironment of the epithelium.
Natural or synthetic biomaterials in the form of hydrogels, such as collagen, gelatin, silk fibroin, PEG, or hydrogels based on decellularized extracellular matrices, are intended to mimic the properties of the extracellular matrix of the stroma. [4-12] These materials can be adjusted to resemble the mechanical stiffness and biochemical composition of the limbal niche to guide cellular behavior and ensure proper integration. On the other hand, biomaterials capable of releasing growth factors or anti-inflammatory agents are also being designed, which actively influence the microenvironment that will improve tissue regeneration. For example, supports that replicate limbal mildness may help keep LEZAs undifferentiated, while more rigid supports will promote cell differentiation when needed.
Small vesicles extracted from cells, the future of regenerative therapies
Exosomes are small vesicles released by cells that carry proteins, RNA, and other molecules, sending repair signals to damaged cells. Unlike traditional cell transplantation, exosome therapies target the microenvironment to promote the natural healing mechanisms of the tissue.
Exosomes derived from stem cells can reduce inflammation, stimulate tissue repair, and improve cell survival. This approach can simplify the treatment process while avoiding cell growth or transplant complexities and taking advantage of the cell renewal properties.
And for the future, what?
Regenerative therapies for the cornea, however, have challenges ahead.
On the one hand, there is still an urgent need to standardise protocols for cell culture and transplantation. Ensuring long-term survival and functionality of transplanted cells also remains an obstacle, especially when immunological rejection is likely to occur.
The dynamic nature of the corneal microenvironment adds another layer of complexity. Chronic inflammation or fibrosis can create an adverse environment that prevents the success of regeneration. Addressing these challenges requires a global approach that combines cell therapy, biomaterials, and specific signaling to modulate the microenvironment.
Thus, successful corneal regeneration requires not only cell replacement, but also an integrated approach that responds to the microenvironment, cell supports, and biological signals that guide behavior. By combining these elements, it is possible to create not only effective therapies, but also permanent therapies.
In summary, the corneal microenvironment is more than a passive área for cellular activity, an active and indispensable regulator of regeneration. Understanding its complexity and being able to reproduce it are the foundation of today’s regenerative medicine.
The bibliography
1.Suanno, G. et al. 2024. “Cell therapy in the cornea: The emerging role of microenvironment”. Prog Retin Eye Res 102, 101275.
2.Assisted by Birbrair, A. & Frenette, P. I'm talking about S. 2016. “Niche heterogeneity in the bone marrow.” Ann N Y Acad Sci 1370, 82–96.
3.In Genna, V. According to G., Assisted by Maurizi, E., Assisted by Rama, P. & Pellegrini, G. 2025. “Biology and medicine on ocular surface restoration: Advancements and limits of limbal stem cell deficiency treatments.” Ocean Surf 35, 57–67.
4.By Fernandes-Cunha, G. According to M. et al. 2022. “Supramolecular host-guest hyaluronic acid hydrogels enhance corneal wound healing through dynamic spatiotemporal effects”. The Ocular Surface 23.
5.It's Lee, Y. According to P. et al. 2019. “Facile fabrication of superporous and biocompatible hydrogel scaffolds for artificial corneal periphery.” Colloids Surf B Biointerfaces 175.
6.Tang, Q. et al. 2022. “Exosomes-loaded thermosensitive hydrogels for corneal epithelium and stroma regeneration”. Biomaterials 280.
7.Feng, L. et al. 2021. “Thermo-Gelling Dendronized Chitosans as Biomimetic Scaffolds for Corneal Tissue Engineering.” ACS Appl Mater Interfaces 13.
8.In McTiernan, C. According to D. et al. 2020. “LiQD Cornea: Pro-regeneration collagen mimetics as patches and alternatives to corneal transplantation”. Screenplay by Sci Adv 6.
9.More places to stay in Chen, F., According to Le, P., By Fernandes-Cunha, G. More about M., In Heilshorn, S. I'm talking about C. & Myung, D. 2020. “Bio-orthogonally crosslinked hyaluronate-collagen hydrogel for suture free corneal defect repair”. Biomaterials 255.
10.According to Li, M. et al. 2023. A "T.E.S.T." hydrogel bioadhesive assisted by corneal cross-linking for in situ sutureless corneal repair. Bioact Mater 25.
11.According to Sharifi, S. et al. 2021. “Tuning gelatin-based hydrogel towards bioadhesive ocular tissue engineering applications”. Bioact Mater 6.
12.Assisted by Sani, E. According to S. et al. 2019. “Sutureless repair of corneal injuries using naturally bioadhesive hydrogels”. Screenshot by Sci Adv 5.
Buletina
Bidali zure helbide elektronikoa eta jaso asteroko buletina zure sarrera-ontzian











