“If when SARS-1 and MERS appeared we had investigated more, today we would be in a better position”
Eleven laboratories in the world work extensively on the covid-19 vaccine. Different parallel strategies are being tested and may be achieved as soon as possible. The biochemist Nerea Zabaleta Lasarte is developing a relentless and full of illusion vaccine in the laboratory of the Mass Eye and Ear Hospital in Boston, with gene therapy. At the same time it is clear: “Along the way many vaccines will fall because they are not very effective, they are too expensive or produce some side damage.” It has provided us with the main keys to the covid-19 vaccine.

Numerous laboratories around the world are simultaneously working on the development of SARS-CoV-2 vaccines: China, USA, Germany, UK… We are seeing different strategies. What can be the most efficient?
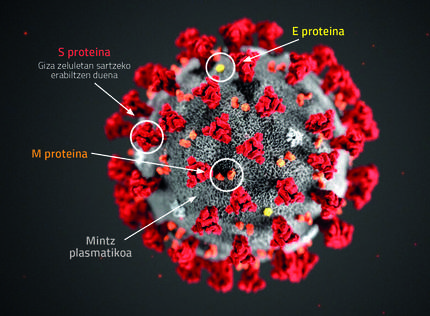
The truth is that we are all using the same protein to develop the vaccine. In a natural infection, a virus protein outside, protein S, helps to join our cells and penetrate them. It is a very visible protein and our organism generates antibodies against this protein, thus obtaining immunity to the virus. So with the vaccine, the same thing: we have to teach the body that protein to produce antibodies. But each laboratory has developed its own strategy to incorporate protein into the body.
One strategy for generating the vaccine is the incorporation of an inactive virus that has all the outside of the virus, but that lacks internal genetic material. Another option is to introduce the protein alone, since in the laboratory it is generated easily. And another option is to carry out genetic vaccines: introduce into our cells a part of the DNA of the virus that serves to produce this protein. In this way, this virus protein would form within our body and generate antibodies. This is our strategy and for this we use the technique of gene therapy: The original RNA of SARS-CoV2 has been converted into DNA and this DNA sequence has been introduced into another virus. We use adenoassociated viruses: small viruses that infect human cells but do not produce the disease. They are natural viruses, but they are very safe. We maintain the external virus canpside, remove the internal DNA and introduce the other virus we want.
There is everything. In China a viral vector like us is being used, but using an adenovirus. Another US group also speaks forcefully of gene therapy, but instead of using DNA, using RNA. They incorporate messenger RNA which is responsible for the coronavirus protein.
How will vaccine success condition the chosen strategy?
Depending on the system we use to show protein S, your body's immune response and vaccine effectiveness is different. It is different to inject only proteins, which are normally injected with an assistant that activates the immune system, or as we teach you within a virus.The vector itself is immunogenic and conditions the resulting immune response.
In addition, the vaccine should get antibodies to the lungs, as the virus actually enters the lungs, never the blood. So even if we have a very strong response and have a lot of antibodies in the blood, if we don't get that response to the lungs, we won't get a good vaccine.
On the other hand, in this immune response, in addition to antibodies, there is a cellular response. They are responsible for the death of infected cells. But it is not the answer that interests us most because we want to avoid the infection itself. This requires antibodies. And this other response, the cellular response, already works when the cells are infected. Therefore, vaccines should get an antibody response.
And is it proven that a system is more effective or must be tested in each case?
No, each vaccine is different and must be tested. But then we have to be practical. A vaccine can be very effective, but difficult to produce. And in order to involve many people, it is necessary to balance the effective vaccine with the simple and economical vaccine to produce.
Fortunately, those who talk about gene therapy are used to generating it at very high doses, and since vaccines require small doses, we believe it will be easy to produce. But we will have to see what the effective dose of this vaccine is.
In fact, once the vaccine has already developed, the next anxiety could be to produce large amounts, such as obtaining masks or respirators, right?
Yes, all of us who are developing vaccines have that in mind and are doing our calculations. It will depend on the effective dose, but we and no one know yet how much we will scale the production of the vaccine.
Will the last vaccine, which will be used for the massive integration of the population, be of a single strategy or fruit of the mixture of all?
The truth is that there is no common test where all types of vaccines are compared, there is no coordination. Each performs its clinical trials and, if it goes well, sells it. Once marketed, it is up to the health authorities to decide which vaccine to deliver.
Our body gets a long immune memory against some viruses, but very short against other viruses such as cataract. What do you know about SARS-CoV-2?
Yes, each virus or bacteria generates a different immune memory. Some produce a very direct and long immunity, which is maintained for years, and others simply respond immunologically to the moment. Normally, before an infection, antibodies form at the beginning of the response and disappear immediately. Once adaptive immunity is created, long lasting antibodies are formed. However, viruses or bacteria of some infections are not able to cause an efficient adaptive immunity, since in the infection there are not enough viral particles or by the characteristics of the infectious agent. In the case of SARS-CoV-2, it seems to generate a long memory, so effective vaccines can be created. At least it should generate enough immunity for this emergency.
It is true that viruses mutate and this can influence the effectiveness of the vaccine, but it seems that SARS-CoV2, for the moment, has not shown high rates of mutation. In the case of the influenza virus it is totally different: it has its genetic material divided into eight small fragments and, coincidentally, if in the same cell two different influenza viruses are joined, these RNA are mixed and new combinations are created. That is, new viruses. Therefore, even though antiflu immunity is maintained from year to year, the virus is different and cannot effectively combat it.
Clinical trials of several vaccines have already reached Phase 2. In order to streamline the process and find out if the vaccine is effective, favorable voices have been exposed for vaccinated people to come into contact with the virus.
This is totally forbidden. The history of science has examples of this, with very serious results. The dogma of clinical trials is to ensure that that person stays the same or better. We broke that dogma. Even a cold. Ethically it's not correct, and it wouldn't be practicable either: to perform a clinical trial we need insurance, and I don't think anyone would ensure it!
In the case of COVID-19 we have the advantage that the disease is spreading rapidly, so there is a great opportunity for the "subjects" of clinical trials to contact themselves with the virus and we can see the results quickly.
Is there a jump step or a strategy that accelerates the process?
For example, having money to investigate is speeding up the process against normal situations.
China published the virus sequence in February and we are already on the clinical vaccine tests. The effort that science is making is unprecedented, at what speed of work is it not?
It is true that there have been many pandemics throughout history, but never in the privileged scientific and health situation in which we find ourselves. The truth is that this crisis has changed my mind. It has been a pleasure to see that in times of crisis scientists have been able to collaborate. It was amazing. There are many people who want to help: “What can we contribute to? they tell us. Our laboratory specializes in protein production. We can help create protein for those who need it and those who want it.” Thanks to this we move so fast. Living has been a privilege.
Will this be a turning point in science?
I think it will leave its mark, it will maintain this special connection that has been created among researchers. If we work together, we share what we know, research advances at another speed. Yes, let it be at a calmer pace, because we work tirelessly: seven days a week, 12-14 hours a day.
And what other things have you learned from this crisis?
I think we have to be aware that past plagues can come back, or at least similar. If after the emergence of SARS-1A in Asia and MERS in the Middle East we had investigated more, today we could be in a better position.
Buletina
Bidali zure helbide elektronikoa eta jaso asteroko buletina zure sarrera-ontzian