Pregnancy in the hands of men

The function of scientists is to ask questions about nature and to interpret and implement their answers. Following the postulate, based on the hormonal changes that women suffer during pregnancy, it was discovered that the externalized hormones inhibited ovulation and launched in 1960 the first hormonal contraceptives for women. After learning about the success of hormonal therapy in women, it was expected to be tested as soon as possible in men. However, especially for socio-cultural reasons, it has taken three decades to initiate more serious research on male contraceptive methods.
In the search for male contraceptives, given the ability to reduce sperm production (spermatogenesis), the first steps were taken with testosterone. Studies with testosterone have an evolution close to 40 years. First of all, in the 1970s, it was attempted to determine the type and dose of testosterone most appropriate to inhibit spermatogenesis. Twenty years later, under the World Health Organization (WHO), the first two multinational studies were conducted to measure the contraceptive capacity of testosterone. However, for various reasons, the results have never been very satisfactory. On the one hand, testosterone, which orally produces hepatic degradation by injection. On the other hand, because it produces important side effects, such as testosterone produces loss of libido and muscle mass. In addition, from the beginning of treatment to effective inhibition of spermatogenesis is a long time (8-10 weeks).
As an example, we must mention the research sponsored by WHO in the 1990s, which was a milestone for the following. In these investigations, a total of 670 healthy individuals administered intramuscularly the enanthate of testosterone (TE) once a week, it was shown that it was possible to maintain spermatogenesis below 3 million sperm per milliliter without producing adverse effects. However, as discussed above, weekly injection reduced retention to treatment. In addition, despite good treatment, the number of pregnancies was significant. As a result, the process of marketing the drug was suspended as a method of contraception.
After the failure of so many illusioned and monetary projects, the investigations stopped. In 2004, however, in the prestigious Journal of Clinical Endocrinology and Metabolism, the results of the trial conducted by Dr. Gu's research team were published with 308 healthy Chinese men through the donation of testosterone undecanoate (TU). TU monthly injections of 500 milligrams showed high efficiency percentages. In addition, unlike research supported by WHO, among those who maintained spermatogenesis below 3 million sperm per milliliter, there was no case of pregnancy. Tolerance to treatment was also very good, apart from the wounds caused by injection and certain reversible adverse effects of low risk (hyperlipidemia, acne, weight gain, hyperhemoglobinemia). However, the good results obtained in China were not achieved with the Caucasians; according to experts, being the most sensitive Asian to testosterone, it would have to use different doses depending on the origin of the individual. Thus, after several studies with TU to measure the effect of ethnic difference on the contraceptive capacity of testosterone, it was observed that azoospermia was higher than 90% among Asian volunteers and 60% in the Caucasians. In addition, we cannot forget that TU is not effective by mouth. Therefore, in the search for more universal contraceptive methods, the doors were opened to new strategies and, in addition to androgens, other hormones were tried.
New hormonal treatments
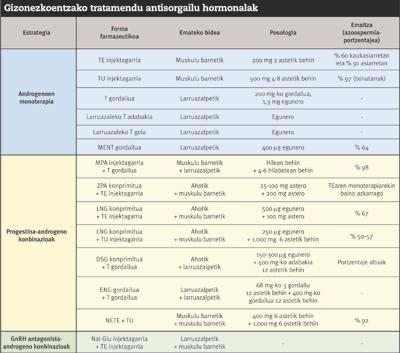
Taking into account the above, it was evident that the hormonal strategy should go another way. For example, to avoid the drawbacks of the injection, they were also tested with testosterone implants under the skin or with testosterone caps and gels on the skin. However, in therapies based on a single androgen, high doses have to be given and they have realized the difficulties they had to control the loss of libido and muscle mass. Therefore, the search for hormonal combinations was used.
Among the candidate hormones to combine with testosterone are the progestins and antagonists of GnRH. These inhibit spermatogenesis avoiding the secretion of hypofisarias FSH and LH. GnRH antagonists are high-power drugs capable of inhibiting spermatogenesis at doses lower than progestins. However, they are very expensive and, since the body metabolizes quickly, they must be injected very frequently. Thus, the researchers' bet was based on combinations between progestins and testosterone.
Perhaps depot systems based on the combination of testosterone and progestins are the best choice in all of them. In 2003, Turner and his collaborators experienced in 55 healthy men the depot system of medroxyprogesterone acetate (progestin family hormone) and testosterone. With this method, placing under the skin the deposit that controls the release of testosterone every 4 or 6 months, the impediments that until then had occurred in the administration of testosterone were overcome. Medroxyprogesterone was given monthly by injection. However, in order to guarantee the total efficacy and safety of depot systems, the investigations carried out are not sufficient.
Currently, progress is made in the search for new drugs to combine with both testosterone and progestins. Among them, the selective modulators (AHMS) for the androgen receptor have been the ones that have obtained the highest results. Like testosterone, AMHS are androgens, but their main advantage over testosterone is selectivity. That is, testosterone acts on many cells of the body and its effects are very general, for example, it can cause the destruction of muscle cells. AHMS, on the contrary, only act on androgen-receptor cells and do not produce libido or muscle mass losses. AHMS are active orally and in rabbits it has been shown to effectively inhibit spermatogenesis without the help of other drugs. However, they are still in the preclinical phase and we do not know if in humans they will get results as in rabbits.

From the 60s to the XXI. After analyzing the evolution until the beginning of the twentieth century, experts have shown that it will be difficult to achieve adequate oral treatment with hormonal therapy. For this reason, since 2004, higher specificity therapies are being investigated based on non-hormonal treatment.
Non-hormonal treatments
Compared to hormonal treatments, non-hormonal treatments, in addition to being able to influence spermatogenesis, are also able to inhibit the function of sperm. In non-hormonal treatment, drugs intended for a specific molecule of the testicles or sperm structure are used. Researchers believe this will prevent the loss of libido and muscle mass that appear with hormonal therapy. However, there are certain barriers to the development of an adequate non-hormonal drug. Among other things, the drug should be able to cross the blood barrier to the testicles.
Many non-hormonal drugs are known that, despite showing preclinically very interesting results, have not evolved by barriers. For example, in monkeys, indenopiridine administered by mouth for 7 days disrupts sperm production for Week 2 without affecting the concentration of testosterone in the blood. In addition, the inhibition of spermatogenesis is capable of maintaining it for 6 weeks, fully recovering for week 16. It is shown that lonidamine (chemotherapy drugs), adjuin and gamendazole, analogous to lonidamine, as well as indenopiridine, inhibit spermatogenesis, making it difficult to function sertoli germ cells in the testicle. However, these three drugs, having a much higher toxicity than indenopiridine, have not advanced.

At present, the specific molecules that control the function of sperm are the ones that are performing the most research. In particular, new strategies are being sought to reduce the mobility of sperm, investigating proteins from different parts of the spematozoid. For example, they have shown that mobility is reduced by influencing the CatSpers cationic channels of the sperm tail of mice. In addition, some cell membrane proteins are being studied, among which the most studied are the adenylylcyclase enzyme and the substituent Na + /K +. However, the results of animal trials remain limited, and it will take a few years to measure the concrete role of these proteins in human sperm, and to know the efficacy and toxicity of these new drugs.
In short, although research on non-hormonal strategies is much more delayed, it should be noted that they must be taken into account in order to avoid the drawbacks of hormonal treatments. However, for the will to become a reality, the interest of pharmaceutical companies will be fundamental.
Buletina
Bidali zure helbide elektronikoa eta jaso asteroko buletina zure sarrera-ontzian











