Amniocentesis, only when they are essential
2014/11/01 Lakar Iraizoz, Oihane - Elhuyar Zientzia Iturria: Elhuyar aldizkaria

“Obtain as much information as possible, with maximum reliability, minimizing the risk for the mother and the fetus.” This is the objective, according to Aloña Elorza, gynecologist of the Zumarraga Hospital, of the screening tests that are currently performed to pregnant women. In these pregnancies are detected with the risk of suffering a chromosomal alteration and the mother is recommended to perform amniocentesis, or biopsy of the placenta, to check if there is alteration.
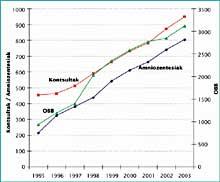
The screening program currently in force in Osakidetza was launched in 2010 and the number of amniocentesis that had been practiced so far decreased by 76.6%: Prior to screening, 19,443 amniocentesis occurred annually, compared to 4,549 in 2010. At present, an average of 1,000 amniocentesis is performed in Osakidetza. For its part, in 2012 the Navarro Health Service announced that each year about 800 amniocentesis is carried out, since in 75% of cases the mother has more than 35 years and in 22% of cases an anomaly has been detected in the screening test.
“When they discover that their child has a chromosomal abnormality, about 95% of women or couples decide to stop their pregnancy. It is a very tough and personal decision,” said Isabel Portillo, head of the Osakidetza Prenatal Anomaly Detection Program. Given that the possibility of interrupting pregnancies is legally authorized until week 22 of pregnancy, in those cases in which the fetus presents some malformation, experts consider it very important that the detection is as early as possible.
The most frequent chromosomal alteration is that of Down syndrome, that is, the trisomy of chromosome 21: According to Portillo, 70 out of every 20,000 children born in the year suffer on average in the CAPV. Along with Down syndrome, the most frequent chromosomal abnormalities include Edwards syndrome (chromosome trisomy of chromosome 18) and Patau syndrome (chromosome 13). About 90% of children with chromosomes have one of the three.
Age, ultrasound, and blood tests
Most pregnant women carry out screening tests in the public health system, according to Portillo: “less than 1% is denied.” The test focuses on three parameters: the mother's age, some measurements of the first trimester ultrasound, and two hormones secreted by the placenta in the maternal blood.
By increasing the age of the mother and increasing the risk of suffering Down syndrome, this was the first criterion taken into account to recommend amniocentesis. However, it is not enough because only 30% of the pregnancies diagnosed with Down syndrome correspond to women over 35.
In the ultrasound of the first trimester of pregnancy, special importance is given to the thickness of the fetus nut fold. This thickness depends on the amount of fluids accumulated in the back of the fetus' neck. For the first time in 1985 it was described that children of a certain thickness have chromosomal alterations. In the 90s, this link was ratified and it was shown that it is possible to detect it also in the first quarter, since the previous ones described the correlation in the ecographic parameters of the second quarter.

In the blood analysis performed on pregnant women in the first trimester, on the other hand, two hormones are observed that secrete the placenta to complete the screening test. They always appear in pregnant women, but it is shown that if there is any chromosomal alteration they appear in the maternal blood at abnormal levels. One of them is beta-gonadotrophine (< -hCG) of the human corion, which usually appears in levels higher than usual when there is a chromosome. The other, the plasmatic protein A (PAPP-A) related to pregnancy, usually appears to a lesser degree when the child has a problem of this type in the blood.
These three tests, performed separately, have little degree of reliability when determining whether the fetus presents any chromosomal problems. The combination of the three allows to determine with a reliability of 90%. The certainty is not total, but occasionally they give false positives and false negatives. The data presented by Portillo shows, for example, that in one year, after the screening of 35,902 pregnancies, they had 205 false positives and 28 false negatives.
In cases where the risk is positive, doctors recommend the realization of amniocentesis, through which it is clarified. In cases where it is negative, however, it is not recommended and in these cases the chances of birth are greater for children with chromosomal problems. However, “in the ultrasound of the second trimester, 70% of them are detected, since children tend to have problems associated with chromosomes; in the case of Down syndrome, for example, they often present cardiac problems, many of which are perceived in the ultrasound,” explains Portillo. The rest are a consequence of the limitations of the test itself, “fortunately they are few,” he added.
Looking for the DNA of the fetus in the blood of the mother
In recent months and years, tests and tests have been launched to assess the risk of chromosomal problems. They work directly with the DNA of the fetus, so they do not take into account factors that increase the risk of suffering from Down syndrome, such as the mother's age.
These techniques are directed to the blood of the mother to obtain the DNA of the fetus. The remains of dead and destroyed cells of the fetus in the lime, including DNA, reach the mother's blood. These techniques are based on the elaboration of fragments of DNA from the chromosomes object of study (in this case 21. They study some specific sequences of chromosomes 18 and 13 and measure how much each of them appears. It is then compared to the average amount that is usually found in samples without trisomy and thus is known whether the amount of DNA associated with a chromosome is excessive or not. The affirmative result would pose a risk of trisomy.
Today, only tests of this type are offered in the private health system. They offer a reliability of 99% and can be made from week 10 of pregnancy, since sufficient DNA of the fetus is already free in the maternal blood. The gynecologist of the clinic Javier Rodriguez Zuatzu values this type of test “very positively”, especially “for its reliability and for not assuming any risk to the mother or to the fetus. Thanks to them we have avoided the realization of many amniocentesis. We propose you to perform the test once the first trimester ultrasound has been performed. It is a very important ultrasound, and if we see that there may be problems in the thickness of the neck fold, instead of performing the screening test, we recommend that you perform the amniocentesis directly, since in these cases it is worth risking. And the new screening tests are expensive, of about 700 euros”.
According to Portillo, “they are other screening tests. They are very new and will certainly evolve. However, at this time the evaluation agencies are subject to study and for the moment do not recommend them as a general screening program.” However, both professionals believe that the future of screening techniques will continue on that path. “For now we have to be prudent and wait. But they are advancing a lot and have a great future,” said Portillo.
When talking about the possible evolution of this type of techniques, some sources also present it as an alternative to amniocentesis. According to Rodríguez himself, “for a couple of years it is possible that through blood tests the entire chromosomal map of the fetus can be extracted.” For his part, the head of the Osakidetza Prenatal Anomaly Detection Program has returned to take prudence before: “It is very important not to confuse citizenship. These news are also screening techniques and I do not think they become diagnostic techniques. In the mother’s blood is the baby’s DNA, but divided, and we do not know if there is all DNA.”
On the other hand, he has defended the screening test that is currently being carried out in the public health system: “The current test is the same one used in all countries and we have to wait for research to move forward to change this test. We cannot jump from one side to the other without knowing that its effectiveness has enough scientific evidence, has a reasonable cost and provides all the information we need or want.”
NOTE (17/02/2015): "Dogma of fetal loss of 1%, decadence", analysis of the risk of fetal loss by prenatal innadador diagnosis, by María Eugenia Querejeta de Policlínica Gipuzkoa, with updated data.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia