The 1918 Pandemic: One Hundred Years of Red today
2018/11/30 Galarraga Aiestaran, Ana - Elhuyar Zientzia Iturria: Elhuyar aldizkaria

According to some sources, the 1918 Spanish flu pandemic was the deadliest of all time. The Black Plague could have killed more people than the medieval Black Plague (which mentions 50-100 million), although in the whole population the Black Plague would be more lethal in percentage. However, it spread all over the world, both in the Arctic and the Pacific Islands, and for the last hundred years there has been no such pandemic.
It was not an epidemic, but a pandemic. Microbiologist Miren Basaras Ibarzabal makes clear what the difference is: “When in a certain time many cases of flu appear it is called a plague. This is common and occurs every year. The pandemic is a global health crisis. It is exceptional and is designated when a large number of infected appear worldwide.”
“In 1918 millions of people became infected and sick and many of them died. What happened? There is a great variability of the virus,” he says.
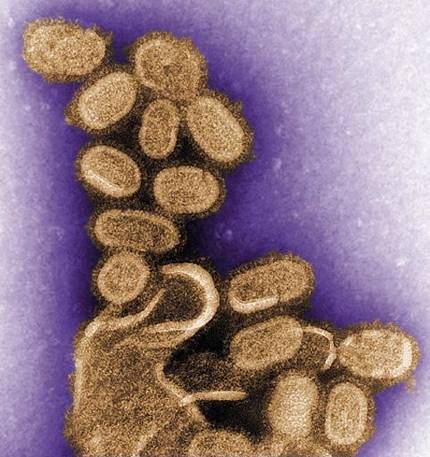
He explains that the flu virus is made up of eight RNA fragments and how different types of viruses are combined. What appeared in 1918 was totally new to the human being.
“Normally, when the flu plague arrives, the most vulnerable are children, the elderly, immunodeficiencies... It also affects healthy people with a strong immune system, but although they get sick, most of the time they don't die. What happens in pandemics? We are all unprotected.” In fact, the virus that spread through birds reached humans in 1918. This type of jumps have occurred before and after. But then it took another measure.
From birds to man
Types of influenza viruses are classified according to the main antigens. The main antigens are hemagglutinin (H) and neurominidase (N). The first has 18 types and the second 11. The virus contains one of these hemagglutinins and a neuraminidase, so the combinations are very numerous. In addition, they can be type A or type B (there is also type C, but they are much less). “We know that all these viruses exist, but not everyone has come to the human being. Most are in wild birds: ducks, birds... There are also other animals, but especially wild ducks. And of those animals you run the risk of jumping the man”, has warned Basaras.
“The arrival of a bird virus to humans, which the recipient did not know, poses a really serious problem, since it does not have antibodies against these antigens.” That's what happened in 1918.
However, seasonal pests are produced by mutation of typical human viruses, the newly created are not so different from the previous ones and people have some protection. “Sometimes the mutation is higher than normal, so the flu that year is usually more virulent.”
To protect against seasonal flu, vaccines are made from the last viruses generated. They usually have three strains: H1N1 and H3N2 type A and other type B. Basaras believes that changes in A are greater than in B and are majority. “Some people think that the vaccine should have four strains to offer more protection, but what is usually given is three for now.”
The cause of the 1918 pandemic was type H1N1. Although at that time it was completely new to humans, it is now quite common and comes to us every year. Among them are other variants of the virus, such as the one that spread in 2009.
Known as influenza A, Basaras has directed: “Influenza A is badly said. The flu is a disease and the virus that caused it was type A, but most are of this type. That was H1N1, but not always, as it conquered part of the genetic material of animals. That’s why it was so virulent and the risk of plague becoming a pandemic.”
He has announced that these events occur once. To prevent risk, there are monitors responsible for monitoring influenza cases, in case of particularly virulent variants, in order to detect and take action as soon as possible. For example, vaccines were created in 2009.
Basaras recalled that there are areas where there is more risk of the virus jumping from animals to humans, as in Asia: “Why? In the nurseries, due to the proximity between birds and people. For example, chicken farms have isolated viruses with H5, H7 and H9. These are not common in humans and have caused several deaths among nursery workers.”
Often these viruses do not spread anymore. In fact, in order for the pandemic to occur, in addition to the virus being antigenically new to humans, it is essential that it be able to transmit it from one person to another, that is, adapt to interhuman transmission. “Because someone may get infected with a virus of animal origin, but if they don’t transmit it they cut off there.”
Multilevel measurements
Basaras has mentioned monitors as a first preventive measure. This surveillance work is carried out in a coordinated manner between international organizations: The World Health Organization, CDC (Centers for Disease Control and Prevention), USA. “When seasonal flu appears, these teams identify and analyze whether the virus is common or not. In most cases it is common and has no special severity. However, viruses that appear off-season and in specific places such as poultry farms can be much more dangerous and it is very important to identify and see them as soon as possible and what type it is and what type it has hemagglutinin and neuraminidase.”
In Europe he recalled what happened in 2016. A virus introduced by wild ducks, type H5N8, caused numerous deaths on poultry farms. It was not transmitted to man, but they had to sacrifice thousands of birds to prevent its expansion.

The surveillance system is therefore the first pandemic barrier. In addition, much progress has been made in diagnosis. New methods of virus identification allow you to know the type of virus that appeared much faster than before. “Until the virus is known, a quarantine is established. There the biggest problem arises when the spring is wild, as effective control measures can hardly be taken in nature.”
Once the virus is identified and when necessary, the next step to prevent the pandemic is the development of the vaccine. Unfortunately, the seasonal vaccine does not completely protect against the common plague, due to the mutation capacity of the virus, and is useless if the virus is new. In any case, whether the virus is seasonal or unusual, there is currently a quick way to get vaccinated to fight it. An example of this was the one that emerged to protect itself from the 2009 flu. Developed by the pharmaceutical company Novartis, production in cellular cultures was key to rapid obtaining, as it is usually done so rather than in eggs.
However, Basaras has recognized that there is still no vaccine to protect against all types of viruses, “and I don’t think it will be achieved in the short term.” However, unlike 100 years ago, in addition to all these preventive measures, there are also drugs to treat patients.”
Usually, after the flu, medicines are taken to treat the symptoms: lower the fever, relieve the headache… However, in most cases they are not taken antiviral because they are not essential, but they do exist. “They are not perfect because they are at risk for resistance, but they can be useful in the risk of pandemic. And in 1918 they didn’t.”
Antibiotics were also very limited and, although useless against the virus, they are useful for treating secondary infections. “Flu patients, if they don’t take good care of themselves, are at risk of acquiring other pathogens, often bacteria. In 1918 many of the flu sufferers died from bacterial infections.”
Therefore, although there is still a risk of pandemic at present, the measures to combat it are much more abundant and strict than at that time. However, experts warn that we must be alert.
For example, in an article published in the journal Frontiers ("Back to the Future"): Lessons Learned From the 1918 Influenza Pandemic) have analyzed the risk of a pandemic today, citing agents that would help spread the virus: climate change (which can affect bird migration), health factors (malnutrition, tuberculosis and malaria, among others), demography… Thus, they estimate that between 21 and 147 million dead.
Basaras, however, is optimistic: “We can now respond in a much more effective way than a hundred years ago.”

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia






