Transplants. Looking back, what?
1991/01/01 Agirre, Jabier - Medikua eta OEEko kidea Iturria: Elhuyar aldizkaria
How things change time. Or more exactly, how you change the way you see things with the passage of time. I keep in mind the news published in its first pages on December 3, 1967 by newspapers all over the world.
At the Groote Schur Hospital in the South African city of Capetown, Dr. Christian Barnard first performed heart transplantation in man. The event had a great success in the media (very understandable, on the other hand), but was also received with great warmth and very good welcome in the most prestigious medical centers in the world.
Since then it has been a long time and today we consider heart transplantation as something quite normal. What can be said from the current perspective? What have things changed? Let's make a historical explanation of heart transplantation.
Historical data
That day, 3-XII-1967, Louis Warkansky, 55, first conquered the heart of another person in the world. Denise Darvall, a 25-year-old girl, died in a traffic accident and her heart lived 18 days in Warkansky's body, while a respiratory infection caused death due to her severe immune treatment.
The first time they worked simultaneously two medical teams in the donor and recipient bodies. While blood pumping in the receptor was artificially maintained (when the heart was previously extracted), with another mechanical pumping equipment they maintained a blood supply in the donor's heart. It must be said, however, that the one who initiated the transplant technique was Dr. Sanway of Stanford University in California, who for the first time described the technique in 1960.
The transplant carried out by Barnard exceeded all medical and scientific limits and was given great publicity to Barnard himself, until he managed to fill a lot of pages of what is called “cardiac press.” Leaving aside all these excuses, the importance of the first heart transplant and the consequences in the sequels are unquestionable.
After the first, heart transplants proliferated all over the world (perhaps something else?) Being more than a hundred those carried out within a year. One of them is the one developed by Dr. Barnard himself to the dental doctor Philip Blaiberg, who survived for 19 months.
However, the history of transplants is older and began more than sixty years ago, experimentally with animals. In the last 20 years, heart transplants have ceased to be a surgical novelty, since every year the lives of thousands of patients can be saved or improved. This spectacular breakthrough is mainly based on the development and fineness of adequate surgical techniques and on the spectacular advancement of the control methods of the transplanted organ immunological rejection. The second factor is especially complex because it consists of eliminating attempts by the immune system to reject foreign tissue, but without the patient being more vulnerable to infection or neoplasia. It is a rather complicated road, as we will see later.
As an anecdote
In November 1978, for the first time in Europe, the transplant of a “heterological” heart was carried out in Nice, a technique put to completion by Dr. Barnard. The patient was inserted in the transplanted heart to keep their own hearts functioning, but functioning less and more slowly so that finally the new heart was replaced.
Robert Dodge, a man who was transplanted twice the heart, was the father of a girl (Sandra Jo Dodge), the first descendant born of a father transplanted from the heart. At the time, the experts surprised the news of Sandra's birth, since the drugs administered to cardiac transplants almost completely destroy the reproductive power of the seed of the patients.
The first combined heart and lung transplant was performed at the University Clinic of Navarra in 1981, 2 years before the same was done in Britain.
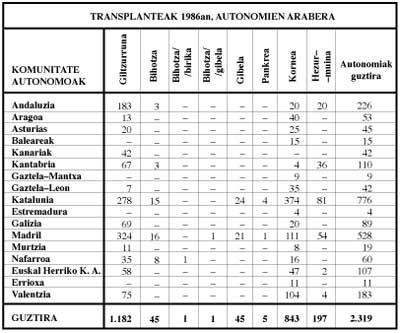
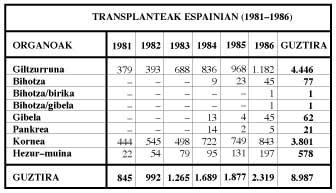
Trasplantes en Spain
In 1968 Dr. Martínez Bordiu performed the first heart transplant in Spain, using the strictly national group (18 September). The patient, 41 years of age, died in a few hours, but this transplant not only increased the fame of the author, then altered for other reasons, but served mainly to demonstrate surgical technique, hospital organization and the value of medical equipment.
On May 8, 1984, there was a leap to ten and a quarter of the night (almost 18 years of leap) in several media outlets, perhaps with advances full of bad intentions and suspicions to find what was called “the first serious transplant in Spain.” Dr. Caralps himself, head of the medical team that carried out the second medical intervention, acknowledged that the times were very different and that the work done by the team of Dr. Martínez Bordiu was perfectly satisfactory and correct, since they were carried out following the techniques, means and medicines of each moment, both the first and the second transplant. At this point, as on many other occasions, history leaves everyone in place.
Problems posed by organ transplantation
The problems are very varied, both technical (currently overcome) and immunological (well known but not yet resolved).
The selection of patients should be careful. The age of the recipient for heart transplantation should not exceed 50 years. As for its level of health, it should not be as deteriorated as to prohibit any surgical intervention, but sufficient to justify the high risk it supports. The disease of the patient should not be greater than 5 years, there will be no significant pulmonary hypertension and by heart failure the hepatic and/or renal insufficiency that all these patients usually have should be minimal.
As for the possible donor, in addition to the medical and legal problems associated with the diagnosis of safe death, you must meet a number of requirements: To be less than 40 years old (from that age coronary arteriosclerosis is frequent); to be known previously the normality of the cardiac function, without infection or any deterioration; that its blood group is compatible with the receptor and that, what is even more important, is assured the histocompatibility between both.
According to the panel of experts at the Stanford University Medical Center, who have closely analyzed the problem of transplants, only 15% of potential recipients are able to accept heart transplantation.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia