Cancer Immunology
1989/10/01 Otsoa Garai, Jorge Iturria: Elhuyar aldizkaria
Irradiation, for example, kills rapidly reproducing cells. Unfortunately, it destroys both cancer cells and light growing healthy cells (bone marrow, epithelial). Drugs,
in addition to eliminating cancer cells, produce unwanted actions such as immunosuppression. Consequently, in immunosuppressed patients (patients without defense systems) the risk of infection increases considerably. Surgery,
finally, is not as fine as the others, so it is very limited in cancers dispersed and located in.

Immunotherapy is the anticancer cure, that is, the therapy that the doctor performs with the Immune System. Immunotherapy is characterized by its specificity and effectiveness. Being specific, the Immune System acts exclusively against cancer cells (and not healthy ones). By its effectiveness completely destroys cancer.
However, as the Immune System itself and its ability to fight cancer are thoroughly investigated, we have realized its reduced complexity and effectiveness. In addition, sometimes immune cells perform opposite actions that favor cancer growth.
However, in many cases, immune cells are able to fight cancer in general. Thorough and thorough knowledge of this complexity will help us achieve specific and effective therapy. How? By promoting the Immune System itself or joining two different treatments.
Theory of Immunosurveillance

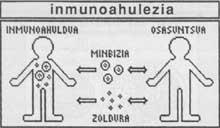
Although the main function of the Immune System is the defense against infections produced by microorganisms, it has another important function as the fight against cancer.
The theory of immunosurveillance explains the mechanism of action of the Immune System to fight cancer. According to this theory, cancer cells appear spontaneously and continuously throughout our body. However, most of these cells do not evolve to developed or mature cancer, since as soon as they appear, the Immune System kills them. Immune cells see newly created cancer cells strange through their surface antigens and then begin to destroy them.
This occurs in the early stages of cancer development, when very few cells form it. Therefore, only cancer occurs in two cases: When the Immune System is weak (this situation is known as immunoweakness) or cancer growth is less than the ability to destroy immune cells.
Despite its appeal, this theory has both contrary and favorable evidence.
Adverse Evidence
* From this theory it can be derived that humans without immune cells should endure a higher number of cancers than healthy ones, since there would be no one who kills newly created cancer cells.
There are mice called “nude” that since birth are not T-lymphocytes. T lymphocytes are one of the most important branches of the Immune System. However, nude mice have no higher percentage of cancer than normal mice.
* If a mouse is injected with a sufficient number of cells extracted from another cancerous mouse, it rejects them. This evidence coincides with the theory of immunosurveillance.
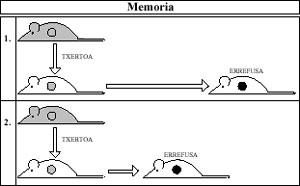
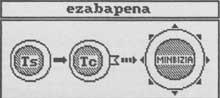
However, if the injected dose is very small, the receptor is not able to reject and eventually cancer cells kill the mouse. This fact is known as “sneaking through” and is that the injected cells are so few that the recipient’s Immune System does not initially detect them. And cancer is very developed for when it detects them.
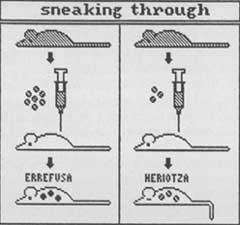
If the theory were true, that is, if the Immune System kills as cancer cells form, it would not be logical for this system to more easily detect and destroy large amounts of cells than small ones.
* For the Immune System to attack and destroy newly created cancer cells, you must observe foreign molecules on its surface. These molecules are antigenic, that is, capable of producing immune response. If there are no foreign surface antigens there is no response.
However, most natural cancers that appear in humans do not contain foreign molecules of the skin. And in any case, these molecules are not able (for various reasons) to produce an immune response.
What is the reason? As already mentioned, the cells that form the Immune System only kill the antigen cells. Therefore, the only cancer cells that survive are antigens, which are those that become developed cancer.
The ability of these cancer cells to prevent the Immune System is called immune escape.
Favorable evidence
* Against what happens in the “Nude” mouse, patients with weakened T lymphocyte function are more likely to suffer from cancer than healthy people. This means that the Immune System plays a certain role against cancer in humans.
A clear example is AIDS. These patients have weakened the function of T lymphocytes, while presenting a fairly high incidence of cancer such as Kaposi sarcoma.
* There are mice called “beige” without NK cells. NK cells are an important branch of the Immune System against cancer.
Mice are more prone to cancer than conventional mice. This evidence favors the theory of immunosurveillance.

* The main problem that arises after transplantation is, logically, rejection. Rejection is performed by the immune cells (mainly T lymphocytes) of the receptor. These cells destroy the inserted tissue after you have seen it strange.
One way to avoid rejection (or at least to reduce the risk of rejection) is to give the patient drugs that eliminate immune cell function. These cells not only participate in transplant rejection, but also act against cancers and infections, so the immunogutxado patient is unprotected.
Therefore, patients who receive the new organ and take immunosuppressive drugs to prevent rejection have greater cancer inference than normal people. This underlines the importance of the Immune System against cancer.
Immune cells to cancer
Although the theory of immunosurveillance remains an unanswered interrogation, we know that the Immune System is able to cope with certain types of cancer, both in its beginnings and later.

a) Specific immunity
Performed by T and B lymphocytes. Both cells need to be previously sensitive, i.e., prior contact with the cancer antigen in order to generate immune response. The two cells, on the other hand, must know the carcinogenic antigen along with the histocompatible molecules. If these molecules are foreign, that is, if the cancer cell is not considered its own, the mentioned immune cells are not able to kill or destroy the cancer.
Lymphocyte B, after knowing the cancer cell antigen (after contact), becomes a plasma cell that produces and secretes antibodies. These antibodies are able to be specially associated with the carcinogenic antigen and through this capacity they participate in actions against cancer:
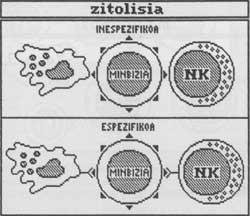
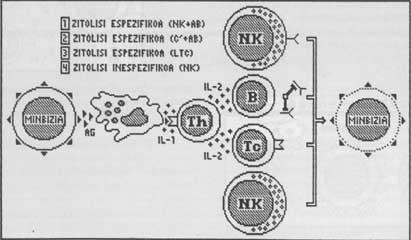
- adhere to macrophage and/or NK cells and perform cytotoxicity by Ab. In this type of cytosis the antibody says what the target cell is, that is, what cell must die. The macrophage cell or NK only makes cylysis.
- are added to carcinogenic antigens on the surface of the cancer cell, which are a privileged place for complement molecules. The complement are plasma soluble proteins. When these proteins bind to the milestone skin antigens are excited and by excitation effect pierce the cell membrane in different places. This causes the death of the target. This type of cytosis is called complement cytosis.
- bind and eliminate carcinogenic antigens that secrete cancer cells present in body fluids. Therefore, antibodies prevent carcinogenic antigens from satisfying T lymphocyte receptors and therefore lose the function of these cells.

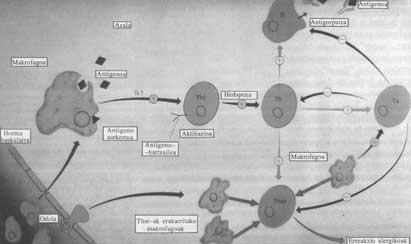
T lymphocytes destroy cancer by cytotoxicity or cytosis actions. These actions coordinate and communicate macrophages on the one hand and the population auxiliary and cytotoxic of T lymphocytes on the other by soluble molecules.
In the first step the cancer cell secretes carcinogenic antigens to the outside. Some of these antigens are captured by macrophages on the membrane, others are captured by cytotoxic T in surface receptors.
In the second step, the macrophage presents membrane cancer antigens to the T-helper and flows interleukin-1 (IL-1). Antigen presentation excites assistant T and causes interleukin-secretions to increase and mature. Interleukins are soluble factors produced and secreted by Immune System cells. They have the function of interacting between immune cells, both exciting and inhibiting.
The T helper is therefore excited by the knowledge of the carcinogenic antigen and forced to grow and grow by IL-1. Then in the third step, auxiliary T secretes interleukin 2 (IL-2) that excites cytotoxic T. As mentioned above, cytotoxic T contains carcinogenic antigens in the receptors.
Finally, in the fourth step, cytotoxic T performs a cytolytic action against cancer cells that have carcinogenic surface antigen. The cylisis mechanism consists of three phases:
- Cytotoxic t knows the target cell (in this case the cancer cell).
- Cytotoxic T secretes cytoolytic substances.
- Cytolytic subjects smooth or kill the target cell.
b) Non-specific immunity
Composed mainly of NK cells and macrophages. These cells do not require predictability, that is, they are able to produce an immune response without prior contact with the carcinogenic antigen. On the other hand, and unlike specific immunity, it is not necessary that its same histocompatible molecules be seen in the cell in order to initiate cylisis. They can kill their own or foreign cells. However, they only act against abnormal cells (such as cancer cells). This means that they know an antigen that is present on the membranes of cancer cells and daring to the healthiest cell. The mechanism of action is similar to the T cells of the specific branch.
However, if the antibodies produced by B lymphocytes adhere to the skin, they act as specific cells and only act against the carcinogenic antigen that caused the production of these antibodies.
Apart from the destruction of cancer, NK cells have the ability to prevent the development of metastases. We have new foci that release metastases from cancer of origin and spread through blood or lymph vessels to different parts of the body. Although in the beginning they are small cell groups, these foci evolve over time towards a developed cancer.
Moreover, NK cells can be excited by IL-2, becoming LC cells. LC cells have an intense chit action.

Macrophages, in addition to their direct cytotoxic function against cancer cells, have a cytostatic effect, that is, they interrupt or stop the proliferation of cancer cells.
On the other hand, as has already been indicated, teaches Assistant T the carcinogenic antigen, which plays an inexcusable duty in the cytotoxic action of lymphocytes.
There are intestinal relationships between specific and non-specific immunity, with the immune response to cancer being a coordinated interaction between both branches.
LT auxiliaries, such as cytotoxic LT, as well as NK cells, or macrophages, produce and secrete substances called lymphokines (the interleukins described above are just a type of lymphoma).
Likewise, antibodies created by B lymphocytes "arm" NK cells or macrophages against the specific antigen.
Macrophages present antigens released by cancer to the LT auxiliary.
Immune Escape
Although the Immune System effectively attacks foreign beings (microorganisms, cancer cells, vaccinated cells), certain cancers prevent the aggression of immune cells by “malicious” mechanisms. The ability to extinguish attacks is called immune escape.
In general, cancer flees when the factors that favor its growth are stronger (more important) than those of the destruction carried out by the Immune System.
Some of these mechanisms only prevent the normal or physiological immune response. Others, on the contrary, also turn off the immunotherapy imposed by the doctor.

The most important are:
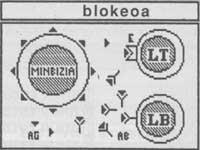
- Sneaking through: The Immune System quickly detects and destroys large amounts of cancer cells. On the contrary, small amounts are easily camouflaged and prevent immune response. Later the latter can become developed cancer. (See figure 1).
- Masking: It consists of a layer that covers carcinogenic antigens by cancer cells (consisting of sialomucin or similar substances). By not being able to come into contact with cancer antigens from cancer cells, immune cells cannot be considered foreign and no responses are made.
- Modulation: Some cancer cells with antigens in the skin internalize these antigens in the presence of immune cells. Thanks to this ability, cancer is not considered a cancer or is attacked.
- Blockage: Cancer cells release large amounts of surface antigens into the environment. These antigens are associated with antibodies produced by B lymphocytes and T cell receptors, blocking both. Thus, cancer cells undergo the two branches of the specific Immune System: the humoral (antibodies) and the cellular (T lymphocytes).
- Inhibition: Some cancer cells secrete substances that inhibit or otherwise alter the immune response (such as prostaglandins). These substances affect immune cells. Therefore, they perform antiimmune action.
- Elimination: There is a population of T-lymphocytes (called T-eliminators) that eliminates Immune System activity. They have the original obligation to govern the immune response to avoid excess immune function, that is, to achieve a balance between the intensity of the strange being and the response. But by eliminating or reducing the action of immune cells they eliminate the wall that hinders cancer growth and promotes cancer development.
Immunotherapy

The general goals of immunotherapy are to increase the patient's cancer resistance and decrease the chances of cancer cell leakage.
There are different types of immunotherapy:
* Specific active immunization: active by compliance with the active need by the patient's Immune System. It is specific because the patient is immunized especially against the type of cancer used in immunization (and not against any other).
It is actually an immunization against the cancer antigen that consists of injecting the patient with cancer antigen extracted from cancer cells. This creates antigen defenses and can hinder cancer growth, as well as being prepared to resist the onset of cancer itself.
The drawback of this therapy is that it is almost impossible to predict what type of cancer the patient supports (except buses). And of course, immunization is not very effective if the cancer is introduced, as the Immune System needs time before starting work (awareness time).
* Non-specific active immunization: it is nonspecific because the Immune System is sensitized not only against the carcinogenic antigen, but against anyone.
Since the response is so broad, that is, it is contrary to such diverse antigens, it is not intense against one of them; in some cases it can slow the development of cancer but never destroy it.
The substances used in this type of therapy are BCG, Levamisol and Poli:A Poli:U.
There are other soluble substances, such as interleukins, interferons, tumor necrosis factor (TNF), and thymus hormones, specific to immune cells that excite cancer but unspecific to cancer. These factors can fight for a long range of antigens, but the immune response is made by certain cells (excited by the factors).
* Passive cellular immunotherapy: it is passive because the patient's immune system does not work. Cellular by lymphocyte action.
It involves injecting both lymphocytes extracted from a sensitized person and laboratory-activated lymphocytes into the patient. Only these “foreign” lymphocytes face cancer.
* Passive humoral immunotherapy: it is called humoral because the patient is injected with humors (molecules dissolved in liquid).
The soluble molecules used in this case are specific antibodies to cancer.
* Immunosuppressive therapy: consists of the administration to the patient of immunosuppressive substances (such as prostaglandins) or immunoweakening agents produced by the cancer itself.
* Corrected chemotherapy: As mentioned, the main drawback of chemotherapy is that chemotherapeutic agents spontaneously kill rapidly reproducing cells. Cancer cells double so quickly that they are the most sensitive cells to these drugs. But these drugs attack healthy cells that reproduce rapidly, such as those in the bone marrow and epitheliums.
On the other hand, antibodies are capable of adhering only to cancer (and not to healthy cells), but not to cell death.

One way to avoid these drawbacks is to combine chemotherapy with immunotherapy. By associating both we associate the antiminvital efficacy of the drug with the specificity of the Immune System.
The technique is to create specific antibodies against cancer. We attach a drug with toxic action to the antibodies in the laboratory. The resulting complex is called “magic projectile.” The antibody of the complex is associated with cancer cells and the drug acts cytotoxic against them.
Although it seems very interesting, this therapy is not as effective due to problems such as the weak bond between the antibody and the cell that breaks easily, the reduced irrigation of the cancer center and the difficult entry into the antibody valley (antibodies reach through blood vessels), the more antigenic modulation (see ahead), the heterogeneity of cancers in different antigenic cells, antigens, antigens.
Adoptive immunotherapy: removal of the cancer patient from immune cells with antivital activity by interleukin excitation in the laboratory and reinjection.
This technique consists of LC (lymphocy-activated NK cells) and TIL (lymphocytes present in cancer) cells. This technique has obtained quite satisfactory results in patients who have managed to eradicate cancer.

Although the ways to fight cancers are very varied, there are very few chancellors. The cause lies in the great heterogeneity of cancers, both in the original organ or tissue (since all tissues of the body can suffer cancer), as in the same cause (viruses, irradiations, chemicals) and in the type of skin or membranous antigen.
Therefore, in the future, therapy adapted to each of them predominates, that is, a special therapy for each type of cancer and disease, in which different treatments are mixed and complemented.
Abbreviations: Ag: antigen (antigen); Ab: antibody; Th: Assistant T (helper); Tc: T cytotoxic (cytotoxic); IL: interleukin; c’: complement (endowment); E: Recipient; Ts: NK: natural killer; LL: lymphokine activated killer; TIL: tumor infiltrating lymphocyte.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia