Heroin: epidemic of the century
2000/03/01 Larrinaga Enbeita, G. | Pineda-Ortiz, Joseba Iturria: Elhuyar aldizkaria

It is not easy to measure destructive effects, but there are statistics that indicate that the aspect is regrettable. Some 1994 data said about heroin use: In Spain and neighbouring countries 0.1% of the total population consumes assiduously and 0.5% has ever consumed it. If we knew how opiates generate dependency, we would know better the processes that are based on the ability to generate dependency on other types of drugs and we can find specific drugs to avoid this dependency.
Composition and use of opium in western culture
Opium is a resin extracted from the fruits of the golden grass (Papaver somniferum) and its main derivative is morphine. In general, the amount of raw opium a sleeping herb plant can give is 5-10 grams. 75-80% of opium are inactive substances and the other 20-25% are active substances. The most important are morphine (10%), narcotomine (6%), papaverine (1%) and codeine (0.5%).
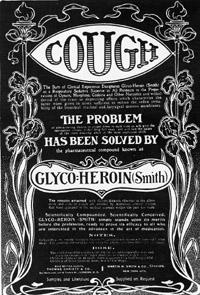
Opium, due to its psychoactive effects, has historically been used in more than any other narcotic, excluding alcohol. Opium has always had a prominent place in medicine, at least in the last 4000 years in therapeutics. However, the scientific understanding of the chemical effects of opiates began with the isolation of the active components of opium. In 1805 Friedrich Sertürner, a German chemist of only 20 years, obtained from the grass of sleep a pure morphine and baptized this substance with the name of morphium, in memory of the Greek god of Morpheus or of sleep. The use of normally pure chemicals has the advantage of being soluble in aqueous and injectable solutions directly to blood circulation. From the year 1853 it was possible to inject morphine, year in which Alexander Wood invented the hypodermic syringe. Through the parenteral pathway, the analgesic capacity of morphine was obtained more quickly and intensively, so this type of consumption (injected) was considerably expanded in the 19th century. throughout the 20th century. The expansion of the British Empire improved trade relations between Europe and the countries of the East that produced veil, while opium consumption in Europe grew. The heroin, founded in 1875, was marketed in 1898 by the pharmaceutical company Bayer as anti-cough, because it was not a generator of dependency (compared with other drugs carrying code). For almost 25 years no action was taken against the use of heroin, perhaps by mouth because cough medications did not expect psychoactive effects to occur.
Currently, the amount of opium that carries the legal means of marketing only reaches half of the world's production. The main producers of illegal opium are the territories of Southeast Asia, known as the Golden Triangle (Laos, northern Thailand and northwest Burma).
Pharmacological Actions of OpiatesOpiates affect living beings through receptors. Receptors are protein molecules that ensure the transduction between excitation and biological effect. That is, the active molecules (called agonists) –neurotransmitters, hormones, drugs, drugs, etc.-, gathered specifically with the receptor, cause cellular change and the associated effect. In 1973 Candance Pert and Solomon H of the John Hopkins University of Baltimore (USA). Snyder found that opioids that were radioactively marked in brain tissues were specifically associated with certain receptors. So far and in this order the m (mu), k (kappa) and d (delta) receptors have been described, as well as some subtypes of them. But beings are not born with morphine inside, so why has our body created these receptors? To answer this question, researchers began to explore natural morphin-like molecules that could form our body and in 1975 discovered two neuropeptides that specifically linked with these opioid receptors: methionine encephalin and leucine encephalin. To date, in addition to encephalins, endorphins and dinorphins have been described, all known as internal opioid peptides. Both these internal peptides and opiates (morphine, etc.) to produce the intracellular effect must be associated with receptors located in the cell membrane. Opioid receptors are bound by G-protein molecules. The excitation of the receptor/G protein system will cause activations and inhibitions of the different proteins (enzymes and ion slots) that make up the effector system. Opiates are primarily responsible for the nervous system, inhibiting or reducing bioelectric activity and the release of neurotransmitters in neurons with opioid receptors. However, the pharmacological actions produced by opioids, both by type and by intensity, are different depending on the opioid class and the type of receptor to which they are associated.

Although opioids bind with the three opioid receptors (m, k, and d), most effects occur through the m receptors. Morphine and heroin activate with great affinity and strength m receptors. Morphine produces a more evident therapeutic benefit, since it is the backbone of analgesic opiates, but heroin has predominated in the last 40 years of this century. Heroin is a semi-synthetic derivative obtained from the addition of two acetylene groups to morphine, which give it a high liposolubility, which facilitates access to brain tissues. For this characteristic, analgesia, euphoria, dependence, etc. produced by heroin. are more intense than those created by morphine. Other types of opiates are now known, including codeine (a natural cough derivative), buprenorphine (semi-synthetic), and methadone (synthetic). The most important pharmacological actions of opioids appear in the central nervous system (CNS). Analgesia is the most known characteristic and we should differentiate this effect from that produced by non-opioid analgesics. Opioids act on the nervous system that transmits pain, especially by relieving the unpleasant and aggravating sensations caused by pain. Other analgesics, such as acetylsalicylic acid, act on the peripheral level and not on the CNS.
Acute opioid poisoning
When the dose of ingested opiates is too high, very severe effects occur. The causes of poisoning are:
- Fortuitous overdose in heroinophanes: it is the most abundant and can be observed in cases such as the adoption of a purer heroin, the miscalculation of the dose, the sensitivity to unconventional opiates (at the beginning of drug addiction) or the usual dose after detoxification treatment.
- Overdose of rejection: it is suicide.
- Clinical overdose: It is observed mainly in children and older people by postoperative analgesia, where opioids are used.
- Unexpected overdose in non-drug addicts: occurs in children after use at high doses of contraceptives or codeine antidiarrheal drugs.
We will always suspect acute opioid poisoning when we observe a triple symptom: coma, myosia, and respiratory depression. The drug used in the treatment of acute intoxication is naloxone. This opioid antagonist prevents the effects of opioid agonists and thus, after passing through the intravenous line, it can be observed that for 2-3 minutes the patient "rises".
Chronic use of opiates
Currently, chronic opioid use can be observed in three situations:
- In heroin addicts: the most common type of consumer is that of drug addicts who support heroin both for play and dependence. According to the latest data, the most common form of opiates is the airway (burning or snorting) and the parenteral pathway is as follows. This trend has to do with the possibility of suffering AIDS from infected needles.
- Patients undergoing treatment: Doctors often turn to morphine to eliminate pain caused by certain diseases.
- In former drug addicts: opioid addicts usually take methadone to quit heroin and remake it. Psychiatrists recognize the existence of two systems of diagnosis of dependence. One of them is the so-called ICD-10, created by the World Health Organization
The DSM-IV carried out by the American Psychiatric Commission, the most used in our environment. The DSM-IV system indicates that drug dependence is an inadequate consumption behavior with psychoactive substances that cause significant deterioration. There are three major pharmacological episodes related to dependence: tolerance, physical and psychic dependence. Opioid tolerance is only the consequence of repeated use of it, that is, the ability of the organism to withstand increasing doses of drugs without symptoms of toxicity.
For its part, physical dependence is an inherent situation in withdrawal syndrome that occurs when the opioid is stopped. Finally, psychic dependence is a conduct based on the urgent need to carry out a harmful action. As far as opioid dependence is concerned, this action aims to cover heroin or other opiates.
Psychic Dependence on Opiates
What best defines drug dependence is not tolerance syndrome and not withdrawal, but psychic dependence. That is, without being able to own themselves, drug addicts have to look for and take the opioid without control and can make it impossible for them to know how long they will suffer without drugs.
Although drug addicts know that opiate use produces physical and psychological effects, they continue to take drugs. Therefore, psychic dependence lies in that uncontrollable need or need for craving. In addition, actions related to obtaining and administering drugs lead opiates to abandon daily activity (work, studies, etc. ).
As demonstrated in laboratory studies, dependence is a consequence of the drug-dependent disease. Continuing with what we have, today we cannot say that drug addiction is a vice, but we must consider the heroin consumer as a sick person. Psychic dependence is a disease caused by three factors, the environment and the type of drugs. Genetic factors can explain the difference in sensitivity between individuals.
In addition, the elements of the environment are made up of objects, situations, living environments and friends related to drug use. These factors are as important as genetic factors, as they prevent drug abandonment after human dependence. On the other hand, psychic dependence is based on different acute effects between drugs and other drugs. Animal studies have concluded that drugs (but not other drugs) produce the phenomenon known as ‘positive reinforcement’. The positive reinforcement system (also called the reward system) is a component that helps living beings meet important needs (food, reproduction, etc. ). At the same time, drugs can stimulate positive reinforcement as if it were physiological stimuli. This system is based on the dopaminergic projections located in the previous section of the brain, the so-called mesolinic and mesocortical pathways.
Physical dependence on opiates and withdrawal syndrome
Withdrawal syndrome is a set of symptoms that occur when a physically dependent drug addict does not receive the opioid. The speed in the symptomatology depends on elements such as the duration of the dependence, the dose of drug used, the administrative frequency, pathologies inherent to the dependence and the type of opiates used. In cases of morphine and heroin, the first symptoms appear within 8-12 hours of the last injection and the total duration ranges from 7 to 10 days without treatment.
For methadone, symptoms appear more slowly and last longer. On the other hand, as withdrawal progresses, clinical manifestations and signs will become increasingly evident. The symptomatology can be classified in three phases: initiation (8-12 hours: rhinorrhea, tearing, yawns, anxiety and sweating), intermediate phase (12-24 hours: mydriasis, hair sedation, bone pain, muscle contractions, tremors, hyperpyrexia, tachycardia, irritability, diarrhea, anorexia and opium, esophageal fever, 24-pimal syndrome In any case, if the opioid is abandoned and rehabilitation is to be performed, it must first proceed to detoxification.
The detoxification action is intended to relieve or eliminate the clinical manifestations that appear as the drug is removed. There are two types of treatment used to relieve symptoms in detoxification: symptomatic (sedative drugs) and substitute (methadone).
Over the past thirty years, numerous research has been conducted on the origin of withdrawal syndrome. As indicated above, a pathological balance is established after a long period of opioid use. Therefore, if the opiate intake is abruptly interrupted, the new balance is broken and withdrawal syndrome is created. Since opiates have inhibitory effects on the brain (especially in the area of the brain stem locus coeruleus), a decrease in opioid use will cause the loss of cell inhibition caused by the drug and the activation of neurons.
Treatment of opioid dependence
As mentioned above, detoxification and treatment of dependence do not have the same purpose. The cures of dependence must adapt to the whole point of view, since psychic dependence is very complex. Addressing the legislation on drug dependence of the Basque Government and the National Drug Planning, all therapies have as main objective to avoid the use of opioids after the abandonment of the therapeutic environment (rehabilitation center or team). In this general therapy, in addition to pharmacological treatment, psychotherapeutic support should be provided to the patient and family until full social integration of drug addicts is achieved. Always keep in mind that there is not only solution for all drug addicts. Therefore, each person and his situation are analyzed. On the other hand, in addition to helping the heroine stop taking opioids, its function is to prevent and treat the pathologies associated with doctors.

Pharmacological treatments are not always essential, but three options are offered if used: alternative treatments, opioid receptor antagonists, and partial opioid receptor agonists. The most socially known and used dependency treatment is methadone. The drug addict is replaced with methadone. Methadone is the complete agonist of opiate receptors, and other pharmacological features are of great importance for its benefits to appear. In fact, methadone generates weaker psychic and physical dependencies. This treatment is usually performed within the Methadone Maintenance Program (PMM). The drug addict, after signing his agreement, will start taking methadone by mouth and within a few months the doses of methadone will be slowly reduced. This PMM forces the drug addict to meet very strict conditions, paying attention to the rules that explain the relationships between the center and the patient. This program allows to control drug doses, frequency of consumption, purity of the drug and associated pathologies (such as AIDS), much better than heroin. Moreover, LAAM (lebo-alpha-acetylmethadol), another opioid receptor agonist, produces effects and mild dependencies. Other treatments include naltrexon. We do not need to confuse naltrexone with naloxone.
Both drugs avoid the effects of heroin and other opioid drugs as opioid receptor antagonists. However, naloxone is used to cure heroin and morphine and naltrexone overdoses helps treat dependence. The advantages of this treatment are the absence of dependency and reinforcement effects and the lack of side effects.
Pharmacological Actions of Opiates
- At the SNC: Analgesia Respiratory depression (due to respiratory involvement) Euphoria Mental and physical dependence Contraceptive force Myosia (pupillary contraction) Nausea and vomiting Neurhonour changes (menstrual, etc.)
- In other organs, appliances, or systems: Constipation Bradycardia and orthostatic hypotension
Acute opioid poisoning
- Neurological symptoms: Drowsiness Seizures Coma (at high doses) Symmetrical myosis Midriasis (pupil dilation) in anoxic state
- Respiratory symptoms: Respiratory depression and hypoxia Acute pulmonary edema
Cardiovascular symptoms:
Hypotension Bradycardia Heart failure and shock- Other symptoms (from false substances): Arrhythmias (by quinine) Severe muscle contractions (by extricnine)
Tribute to David Artola Blanco.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia





