History of Artificial Lactation
1993/10/01 Txakartegi, Xabier Iturria: Elhuyar aldizkaria
Natural Lactation (R.D.) has provided the human being a balanced diet for thousands of years in his early childhood. When the mother could not breastfeed, and this occurred in less than 10%, work carried out by the indúes. Soon after, in the central decades of this century, milk banks were created to deal with the scarcity of the Indians. That is to say, until it entered this century there was no safe alternative for child feeding outside the R.D., and very few children survived by feeding during the first year with breast or nurse milk. To realize this, just look at the table (Table 1).

Although infectious diseases were one of the most important factors for infant mortality, the known statistics show a tremendous mortality in children fed without breastfeeding, as can be seen in the table.
The discoveries in biology and medicine at the end of the last century laid the basis for the production of the representatives of Human Milk: the composition of the different types of milk was determined, the benefits of pasteurization were known, and the child's nutritional value was attributed to heat-treated cow's milk. At that time, there were already doctors looking for representatives of the O.E. (breast milk). In the early years of this century, in some clinics and in some cases, cow's milk was added to R.D.
Soon after, in the 20s and 30s of this century, the food industry began to manufacture artificial milk by changing cow's milk. In the years mentioned, both the percentage of R.D. As its duration diminished remarkably in the rich countries. Bottle lactation is imputed to the scientific value provided by certain physicians. During World War II and in later years it was a recovery of D.N.I., but it is not difficult to see that the lack of raw materials and money was the cause. From the decade of the fifties, the decline of R.D. It occurred in the industrialized countries, reaching the minimum at the end of the 60s and early 70s. In 1972, only 20% of American mothers left the hospital feeding their baby with breast milk; in Sweden, in 1971, of the total children of 2 months, only 30% and 6% of those of 6 months were fed from R.D.
N.V. the reasons for separation, in mother-child interaction, should be sought in the opposite effects that have produced the evolution of modern society. Among them, rapid disordered urbanization, overpopulation, environmental pollution, the incorporation of women to work, the improvement of maternal education, the modification of the concept of family unity, emigration, the non-study of lactation, etc. Of course, doctors have also been guilty because they have considered and recommended breastfeeding through the bottle as something scientific.
These trends were first exported to the Eastern European Countries and later to developing countries. And the urban nuclei of the latter are, at present, the places that are most gravely found in the problem of the fall of N. In many states, the downward trend of R.D is being observed. in developed countries until the 1970s.
The most widespread opinion until the 1970s, E.N. The loss was the logical consequence of the modernization of lifestyles. At the beginning of this decade the irreversible trend was questioned and associations began to be created in favor of feeding breast milk in the Western industrialized states. In 1956 the “International Milk League” was created in the United States. In any case, we must take into account that since the end of the last century the R.D. that were created by associations of women, mothers, doctors, etc. The “Movements of Return to Nature” of the 60s and 70s also in the Basque Country. They tried to drive him.

The United Nations Consultative Group on Protein and Calories (“PAG”) developed intense and profound work between 1956 and 1977, recognizing the E.N as a mandatory measure for public health to avoid poor child nutrition. Promotion. He warned of the negative consequences of the inadequate promotion of artificial milk produced by children's food industries. In 1974, the World Health Conference called on governments to enact laws for the production industry of Artificial Milk to limit its commercial propaganda and improve the situation of working women to breastfeed their child. Other institutions such as UNICEF, FAO, ILO, International Association of Pediatrics joined the defense of Mother Milk (A.E. ).
The World Health Organization (O.M.E. ), which currently has a large participation in the promotion of the E.D., has launched a series of studies that analyze how to develop programs for its impulse. To clarify its position, the O.M.E. Feeding to the Breast and Small, carried out in October 1979, says: and the joint demands of the U.N.I.C.E.F. In his first point: “Inadequate food practices for infants and their consequences are one of the most important problems in the world and are becoming a major obstacle to social and economic development.
Given that to a large extent it is a problem created by the human being, we must look at our science and technology on the one hand, and at our social and economic structure on the other, as a responsibility that must be reproached and as an action that covers the great achievements in development.” It is currently demonstrated in R.D. and that modern and industrialized society is compatible with the sensitivity and social support of the needs of mothers and children.
Responding to the above, both in the percentage of R.D. As in its duration, its recovery has been achieved in the developed world, although in no case has the percentages of the second decade of the present century been reached. Scandinavia is the region that most approaches its previous percentages, similar to that of 1945. The promotion and recovery of the R.D. In that region it began before the issuance of the International Recommendations, and the following reasons are usually highlighted to understand its success:
- Information to individuals and private associations who subsequently obtained support from governments.
- Recommendations of the International Professional Organizations, Governments and Medical Societies.
- Social support that the family has received.
- Change the “rooming”, that is, the opinion on the feeding of the newborn in the slaughterhouses, and apply firmly the advice on the trend of the A.E.
- In the decade of the seventies a critique arose against advertising in favor of the substitutes of A.E. that allowed the industry to make much less advertising.
- Extension of the duration of maternity leave: Although in 1955 it was 3 months (in addition to 80% of the salary), in 1974 it was extended to 4 months, in 1977 to 7 months and in 1980 to 9 months of work rest, both maternal and paternal (Sweden).
Behind the Scandinavian countries are the industrialized ones of Oceania in the recovery of the E.N. and later the other developed western countries.
As has already been mentioned above, the developing regions are currently facing the biggest problem, especially in their urban areas, where there is a sharp decrease in the percentage of N. The use of A.E substitutes. It is accompanied by many problems. The lack of health, the poor washing of bottles, the high price and the lack of control of the administration, among other factors, have increased the rate of disease and mortality.
The O.M.E. divides the States and social groups of the world into 3 large groups according to the situation of the A.E. or the phase in which it is situated:
- The first phase is traditional and the percentage and duration of the A.E. They are high.
- The second phase is transitional, with a percentage decrease and a reduction in duration.
- The third phase is recovery, with percentage increases and duration.
The countries, as well as the different subgroups of population within the country, have these phases at different times. The first group to influence change (both enlargement and reduction) is usually an urban elite, that is, a social group and above all a cultural high level. The group that follows is the poorest citizen. The last group, which has the least force to change, has traditionally been agricultural. The national index of R.D. will increase or decrease according to the phase in which each group is located. To realize this is appropriate this image made by O.M.E. (Figure 1).
The figure shows that there are 8 stages according to the R.D National Index. and of the population subgroups. To clarify better we will say that in the first group is Zaire, in the second Nigeria, in the third, in the fourth and in the fifth, Philippines, Brazil, etc. ; the sixth Basque Country; the seventh United Kingdom; and the eighth Sweden.

As for our environment, at the end of the 1970s, 61% of children had R.D. in the Spanish state, and at 2 months only followed 28.7% of them. In 1980, DNI. 84% had it and at 2 months remained 73.2%. It seems that after recovering, there is a stop in the Spanish state, or the recovery is no longer perceived. In fact, at present it is observed that in the R.D. A takeoff occurs of 60-80%. If at 3 months continues 20-40% with I.A., at 6 months only 6% is reached.
However, the differences are remarkable and in some cities a great growth has been observed in recent years. In Madrid, for example, the average duration of 2.5 months of R.D. From 1976 has climbed to 3.4 months in 1990. Or a study conducted in Gades shows us that they have a prevalence rate of 42.6% in the 5th month, but especially in recent years have been those who have experienced a more remarkable increase, supposedly thanks to the Basque Studies Program. Another study in Gran Canaria reveals that between 1988 and 1991 there were prevalence rates between 81.8% and 71.27% of 3 and 6 months. But not everything is ascension. According to statistics compiled by the Municipal Vaccination Program of Barcelona, the prevalence rate of 2 months is 25% because the average duration of the R.D. is very low.
As for the Basque Country, in a study carried out in 1985, it was observed that the percentage of mothers starting with R.D. is 73.2% (when leaving the hospital), while mixed lactation reached 83.9%. At three months 57% and at six months 19% continued to breastfeed, representing 47.8% and 15.9% of all mothers (Gipuzkoa).
In a multicenter research conducted in the Bizkaia region in 1992, prevalence rates of 41% and 13% were detected for 3 and 6 months. In another study, also from 1992, working with samples obtained from 13 pediatric consultations (representative for Bizkaia), it was observed that those initiated with R.D. were 82% (the percentage is 72%). when we speak of emptiness). According to a study carried out in Vitoria-Gasteiz, the percentages started with R.D. They are 83% and 92% for average and low socioeconomic levels, the prevalence rates of the 3rd month are 63% and 38% and those of the 6th month of 29 and 11% for these social levels.
According to the study carried out by us in the City of Gernika on R.D. 1984-1989, the average duration is 3.4 months, being 2.61 the first year and 3.52 at the end. Prevalence rates for the third and sixth month are 54% and 21.8%. They are high when we compare them with the rates of the area and some states (Spain, USA or Great Britain), but they are far from those they get in Scandinavia, for example. According to this study, mothers between 21 and 35 years old, those who have university studies, those who work in the countryside and those who live in the neighborhood. On the contrary, statistically, mothers under 21 years of age and with a very low level of studies are much less.
Prehistory PrehistoryOrphans of Paris (1771-1777)Orphans of Dublin (1775-1779)Orphans of London
31.00010.272- - -25,000 (80%)10.227 (99.6%)- - (90%)Table 1. N.V. mortality of unnourished orphans in the eighteenth century.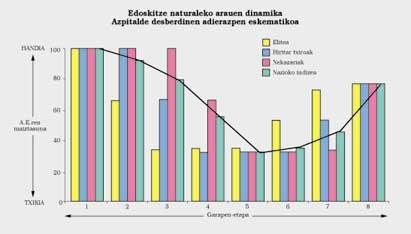
Note: Note: To see the last photo well you can go to the pdf.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia





