Alternative Treatments for Chronic Kidney Failure: Better Transplantation
1989/12/01 Ibarguren Olalde, Karlos Iturria: Elhuyar aldizkaria
The heart has always been regarded as an important organ of our body, as an organ that maintains life. If the heart stays, life ends. The first thing that occurs to us is to analyze the pulsations or pulsations of the heart to know if someone is alive or dead. Certainly the importance of the heart is total, but there are other organs as important as the body itself: the central nervous system, the liver, the lungs and, of course, the kidneys.
The latter have, if necessary, a peculiarity that others do not have. Man has got a machine that can do his job: DIALYSIS. There is a machine that can do the work of the heart, but besides being very large, some problems still unsolved do not solve the problem of people who need an artificial heart. In the case of the kidneys the results are better, but as we will see, patients have to pay an expensive price to continue living. As a result, and as in other organs, the most appropriate treatment is transplantation, in which all of us can play an important role through OUTCOME.
Chronic kidney failure
The main function of the kidneys is blood cleansing. Metabolizing substances entering the body through food produces a number of waste. The kidneys are responsible for their expulsion. The more damaged, the less waste they remove and the more waste they accumulate in the blood.
The most dangerous substances that accumulate are Urea, Potassium and Creatinine. If they reach a high degree of concentration they can cause death, but before reaching it some symptoms begin to appear and their set is called uremic syndrome.
In addition to cleaning the blood, they have other functions. These include the synthesis of the hormone ERYTHROPOIETIN. This hormone causes the formation of red blood cells in the blood. Consequently, anemia and its consequences must be added to the symptoms of insufficiency. Recently this hormone has been marketed and, despite its high cost (around one million euros per year for each patient), it can reject the transfusion problems necessary so far.
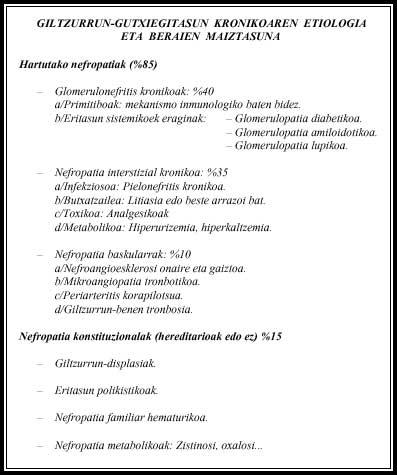
Many diseases can cause kidney failure (Table 1). Some of them are hereditary, so several members of the same family may be ill.
Initially the symptoms are very nonspecific: vomiting, discomfort, hypertension, fatigue, etc. Blood and urine tests may suspect something is wrong. Other tests will then be done to determine whether or not the affected are kidneys and, where appropriate, the cause of the damage. This can happen to anyone and by then it can be too late; within the dialysis world we will find ourselves a little sooner or later.
Dialysis
The chemical bases of dialysis were established by Scottish chemist Thomas Grahan, but medical applications come from researchers Wegner, Starling and Putnam. The latter, as a result of research carried out around 1922, became aware of the importance of the membrane called peritoneum that surrounds the intestines in solving this problem.
If liquid was inserted into the abdominal cavity, in about three hours it was balanced with the blood. It seems that the first person who applied this technique in a patient was Dr. Ganter.
From the blood of a person suffering from chronic kidney failure, in addition to urea, creatinine and potassium, water must be excreted, since the kidneys cannot remove the drinking water. To do this, the liquid that enters the abdominal cavity is scarce in the substances that we want to remove from the blood and also hypertonic with the blood to pass from the blood to the liquid.
In 1913 John Abel and his collaborators took the first steps of what would later be hemodialysis. In this experience he used as a base for dogs without kidney. He took blood out of an artery and after passing it through a machine that “cleansed” them into a vein. In this machine the blood and a liquid as I mentioned above were put in contact separated by an artificial membrane, passing waste and the excess water from the blood to the liquid. On February 18, 1926, Dr. George Haas first applied to a person.

Although the technique has improved substantially, the foundation is the same and the types of dialysis currently performed are two: Peritoneal and Hemodialysis.
Hemodialysis
As already mentioned, this technique consists of blood extraction and reintroduction to the body after passing through the “artificial kidney”. Two needles are inserted into the patient's vein, one for blood extraction and one for introduction. For this it is necessary to perform a “fistula” in the patient’s forearm. This fistula is only the direct connection of an artery and a vein; for three or four weeks, the caliber of the vein will increase considerably, so the flow that will flow through it will facilitate the process.
The blood looks strange the walls of the artificial kidney, so the blood is cooked and of course does not circulate. To prevent this, an antigen called “Heparin” is added to the blood. This process also has its risks. If it gets too much, it would cause bleeding in the patient and vice versa, if the blood went inside the machine, the patient would lose about 300 cubic centimeters.
Although the technique is the same, hemodialysis can be of four types. If the patient is uncompensated (i.e., his blood is “very dirty”), it should be done in the hospital. Once compensated, you can perform home hemodialysis, in a club or self-service. Doing at home has as main advantage freedom with the hospital. However, you need space and someone in the family should help you (of course, you have to learn the process), but psychologically it is a great advantage for the person. Going to a club is easier than going to the hospital. In addition, the risk of pavement is lower. However, in the Basque Country there are few who dialize at home and there is no dialysis club.
Peritoneal dialysis

In this technique, blood and dialysis fluid come into contact through the peritoneum. Peritoneum is a double membrane that collects the intestines and other viscera of the abdominal cavity. Due to the abundance of blood vessels, there is a large relationship between blood and dialysis fluid. To be able to insert fluid into the abdominal cavity, it is necessary to place a catheter that communicates the skin with the abdominal cavity.
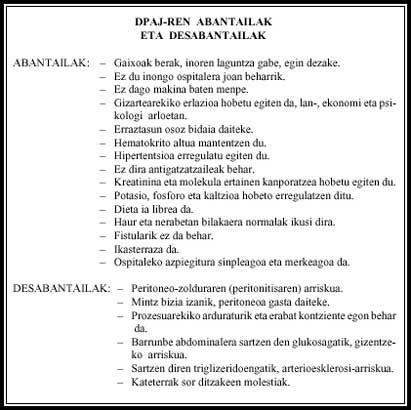
The patient enters fluid, leaves about six hours, and once removed, the patient enters a new fluid. Each change process lasts approximately half an hour and is performed four times a day. Dialysis is continuous and no harmful substances build up in the blood. This process can be performed by the patient without help. Despite the great advantages, it has other problems (Table 2).
It must be said that Gipuzkoa is a pioneer in this technique. Of the 180 people included in the dialysis program in this province, about ten are in the predialisis (with fistula practiced and to be expected to start dialysis), about 31 in continuous peritoneal ambulatory dialysis (DPAJ), about four in home hemodialysis and the rest in hospital hemodialysis. Every year in Gipuzkoa about 35 new people join the dialysis program.
This percentage is similar in other countries: 50 people per million inhabitants. The longest on dialysis has been 16 years. Although the mean age of patients is about 40 years, there is an important group of 18 to 25 years.
Problems
As seen so far, understanding that dialysis has many problems is not difficult. These problems are not limited to medical but also social and psychological. If the treatment is done in the hospital, they must go three times a week and stay in it for about four hours tied to the machine. If we add the controls to which they are subjected (analysis and other tests), it is evident that they have problems to work in the workshop and that therefore they are the first to go to the street when there are incidents in the workshop.
At the biological level they also have important problems. Their sexuality is limited, lack of initiative and, if necessary, strength to practice sports, and they have to take into account food (especially water, sodium, potassium and protein).
The food problem is terrible, more in a society like the Basque. Our eating and drinking habits are really harmful. If necessary, the biggest problem is potassium. This ion, so abundant in most fruits, can paralyze the heart and therefore kill the person.
The problem of liquids is not a joke either. In the face of the heat and feeling of thirst of summer you can not drink anything and when all friends are txikiteando have to enter the bar and be watching, they are not liked by anyone.
Work mistakes, dependencies with other people, lifestyle changes, etc. have a great psychological influence. Even more so if the disease has led the patient to perform hemodialysis in a short time. If the process has been gradually implanted and the patient has had time to become better aware, accept.
Although the personality of the person before the illness is very important, there are factors that make problems worse, such as adolescence. At this time the person has not organized life, but at the same time has a lot of projects and ideas for it. The disease totally conditions these situations, progressively limiting the illusions of the teenager.
All this causes in the patient a state of stress, anxiety, nervousness and irritability. Chronic patient status accentuates this situation, pushing a cyclical situation marked by depression, weakening and lack of projects and interests.
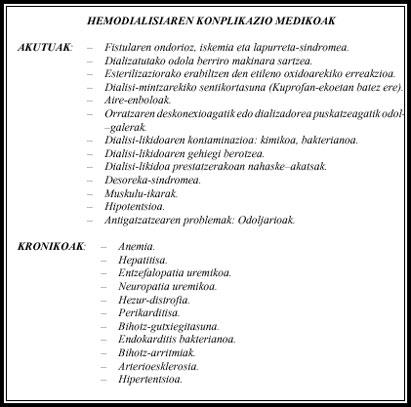
There are also few somatic problems that occur at the medical level. These may be for the moment or chronic (Table 3).
Transplant
As mentioned above, this treatment is not definitive for half of patients on dialysis. They are the subject of transplantation. As we will see, even if it is not the panacea, at present the best treatment is certainly the transplant.
The biggest problem to overcome is rejection. It may be acute or chronic. While the former forces the restitution of the organ, chronic rejection can live for several years, until the kidney that has suffered the rejection returns to the insufficiency. The threat of rejection is constant and whenever they have to make another analysis, fear always exists. The highest risk of rejection occurs during the first year (Table 4).
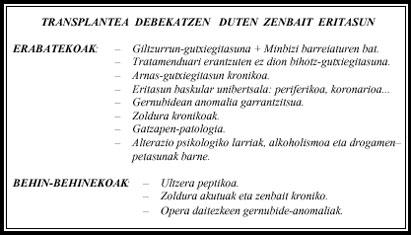
As the body sees the new kidney strange, its immune system will attack it. To prevent this from happening first, it is necessary to analyze the compatibility between the donor and the recipient, that is, if there is a same blood group and a similar HLA system. The greatest similarity occurs in twins born from the same oculus. Therefore, there will be no rejection between them. The similarity between members of the same family will be greater than those of the outside. When rejection appears, the pathway of improvement is that of drugs; the stronger the rejection, the more dose. Because most drugs have side effects, and given that treatment is lifelong, they cannot be forgotten. Recently, a drug called cyclosporine has been marketed with better results. Although problems are being overcome in these years, we still cannot forget them at all.
The transplant may be of two types: you can catch the survivor's kidney or the corpse. The first case occurs in very limited situations, when the patient will die or similar. In the second case, the law requires that the death certificate be signed by three doctors, twice and after having completed all the necessary studies to confirm the death of the person for 6 hours. Given that the kidney "deteriorates" immediately after death, there is little time left to proceed to extraction. Therefore, in order that in such a short time relatives are not forced to make this decision, right now we have to say that we are donors.
The advantages of the transplant are clear: the patient gets the freedom of the machine, its general condition improves a lot, does not need transfusions or erythropoietin and its socio-psychological situation improves markedly. With some limits, the change goes from being sick to healthy.
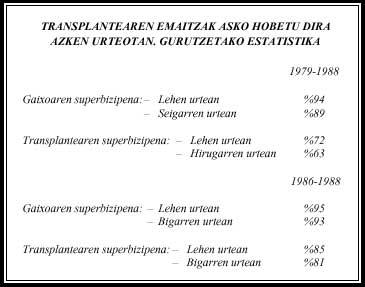
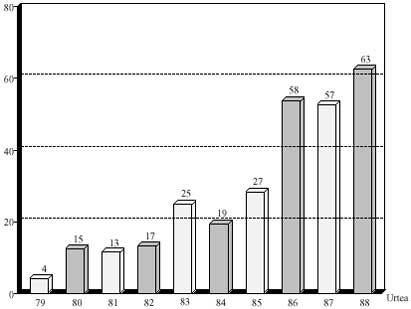
In the Basque Country, transplants are nothing new. In the specific case of the Gipuzkoans, before they came to Pamplona. They are currently held in Cruces de Bizkaia. If we analyze the results we can observe that the technique has improved a lot (Table 5). At this time in Gipuzkoa there are about 90 transplants and one of them has 10 years with a kidney that is not his. Here very few have been made with the kidney of the living person.
And what if there is rejection? The consequence may be death of the receptor or loss of the transplanted kidney. In the second case, the patient returns to dialysis, but the possibilities of a new transplant are maintained. A maximum of three are considered to be possible. In the Basque Country, the second transplant has already been performed in a patient who has suffered the recusal.
Cooking
About 14 years ago the ALCER association was created in Gipuzkoa to respond to the demands, concerns and problems of patients suffering from chronic renal failure. This association can be defined as a group of renal patients. At that time their requests were concrete (that all patients had a dialysis machine, that the displacements were free, etc. ). ), currently and as the required things have been achieved, their work has been changing: they organize campaigns in favor of kidney donation, distribute the donor card and take control of them... but, if necessary, their most important job is to offer patients comprehensive care that responds to psychological and social problems that institutions have not yet solved. Currently the municipalities of Gipuzkoa, Bizkaia and Araba are part of the ALCER-EUSKADI Association, while Navarra has sought contact with Aragoa.
Note:
Many of the data presented here have been provided by Kolde Narbalaz and Xabier Irazusta of the ALCER of Gipuzkoa. Thank you for your collaboration and advice.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia



