On the way, stem cells
2012/04/01 Roa Zubia, Guillermo - Elhuyar Zientzia Iturria: Elhuyar aldizkaria

UPDATE: Macchiarin, denounced and published for fraud in 2017
In November 2011, a 30-year-old American patient, Christopher Lyle is transplanted an artificial trachea. Lyle had very advanced tracheal cancer and it was not possible to operate. His only healing option was a trachea transplant that was facilitated by a team of the Swedish Karolinska Institute. "It's a second chance for me," he said.
For him, it was an opportunity to continue living and for scientists, test a new methodology, since transplantation to Lyle was not in any way.
They did the trachea "from the ground up", that is, without having to pick up a donor. Instead, a synthetic structure was manufactured. Lyle measured the exact dimensions of the trachea and began manufacturing. The basic structure of the trachea, an empty support, was manufactured at the University of London, modeling the proper shape with nanofibers of the PET polymer. And during the construction of this basic structure, the American company Harvard Bioscience prepared a bioreactor, a special container to form the trachea.
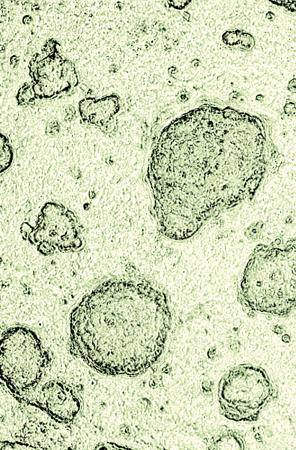
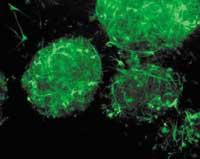
The synthetic structure of the trachea was introduced in the bioreactor, along with stem cells taken from the bone marrow of Lyle, and was constantly moved for two days, as the turns are given to burn the chicken. "We need almost 36 hours for cells to cover the entire structure," explains the surgeon at the Karolinska Institute, who has transplanted Paolo Macchiarin. And during this time the stem cells worked as expected by the doctors. They joined the structure, began to form new cells, and the walls of the trachea were formed around the basic structure. Within two days, the doctors had the complete trachea. He was then transplanted to the patient.
Short term success

The media have praised this methodology. It is actually the second transplant of this type. The first was done by Macchiarini himself, but from another starting point: the basic structure of the trachea was formed from the trachea of a dead donor, to which most of the cells were removed until leaving an empty support. The rest of the process was the same in both transplants and the result was satisfactory in both.
However, the Macchiarini team still has no perspective of years to properly assess these two tracheal transplants. To be able to talk about success, you have to wait a while to see if the new organs give problems or not. The condition of the trachea should be observed at least five years, and should be checked if the transplanted cells of the trachea have been replaced by others produced by the body. The success of a transplant has a lot to do with its duration. However, for the moment, Macchiarini's team is optimistic, and its methodological benefits and advantages are very remarkable.
To complete the walls of the new organ, it has been worked with stem cells of the patient, which solves many medical problems in the usual tracheal transplants. The first is to avoid rejection of the organ, one of the main causes of stem cell therapies. In this case, the body does not consider the cells of the new organ strange, and the person receiving the transplant should not take anti-rejection medications. In addition, the method solves the problem of infections. In conventional transplants, to avoid rejection, doctors weaken the immune system, increasing the risk of infection. In fact, many trachea transplants fail due to bacterial or viral contamination. "The trachea is in direct contact with the outer part of the body," explains Macchiarin. "Every time we breathe, the air -- clean or dirty -- passes through the windpipe. And in transplants with synthetic tubes covered with stem cells, in the future there are no infections".
Another of the main advantages is time. If Macchiarini's methodology is based on a synthetic support, the presence of a donor is not necessary, which directly affects the transplant period. In Lyle's transplant, "adding all the time, we have been two weeks from the beginning until we were able to transplant," explains Macchiarin. "By the usual method, we should wait for a donor and it is not possible to predict when the donor will appear. With this method, however, we can perform a rapid transplant to a patient with a tumor."
And they have achieved it, but Macchiarini has clear that these transplants are still of investigation. "So far we have only proven that this methodology works in two patients, we cannot stay there." At the same time, he wants to highlight the practicality of work. "I am not a researcher, but a clinician who does research, and in addition the research I do will be used directly by patients. We are ethically forced to do things in the simplest way possible to make it possible throughout the world."
From the economic point of view, for the moment, they are very expensive transplants, Lyle had to pay approximately 350.000 euros for the whole process. But the transplants made are no more than the beginning of the track.
Transplant or regenerate
Where does this therapy lead? To what extent is a revolution expected? From the medical point of view, the process is not completely rounded. "Problems still arise," says Macchiarin, "but if we continue to investigate, I think we're going to turn it into a standard technique."
The change that can mean the results of the research can be very varied. The creation of bespoke bioartificial organs will not be mandatory. Macchiarin sees another future: "Instead of growing in vitro stem cells, why don't we turn our own human body into a bioreactor? For example, if in an operation there are regeneration problems, we can add stem cells and add growth factors to accelerate regeneration." This idea is also applicable to the field of transplants. Therefore, to the question of whether stem cells are going to be a revolution, Macchiarin answers: "I think they are not going to revolutionize the technique of transplants. How will we treat an affected function? Through a transplant? No. On the contrary, stem cells of the patient can be used to recover this function. That is feasible, and that will be a radical change in the field of medicine."
The regenerative medicine of organs or tissues generates a great hope for the future. But some experts believe that this medicine will never be a substitute for transplants. One of them is Rafael Matesanz, president of the National Organization of Transplants of Spain.
"The line of stem cells is called regenerative medicine and, as its name indicates, its ultimate purpose is the regeneration of affected tissues or organs. They try it with heart cells, but - explains Matesanz- without great success. People who have suffered an infarction, for example, are injected with stem cells from the bone marrow into the myocardium to regenerate the tissue, since although the infarction itself has treatment, the lesions it leaves no". This treatment can be tissue regeneration. "It has great potential," says Matesanz, but also great limitations. "This will only be possible in tissues. It is done to treat severe burns, using skin stem cells, keratinocytes. But one thing is the regeneration of a piece of skin and another the regeneration of an entire organ, such as the liver or the heart."
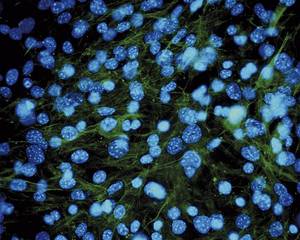
With stem cells, three levels are worked. The first is what they do today, that is, the introduction of cell therapy in certain processes. A damaged tissue is added stem cells in the hope of regenerating it. It is a very limited technique, it only works in a few cases. For example, it is used in corneal limbo transplantation and other small therapies, but for the moment it has no great guarantees.
The second level is the reconstruction of the epithelium to empty organs by stem cells. Macchiarin's transplants are an example of this. "What they've done is a very good idea, but it's just a beginning," says Matesanz. "I'm not going to say that's simple, but today you can do it with technology."
And the third level is the formation of complete and functional solid organs. They are bioartificial organs and some trials have already been conducted, but they are not usable for transplants. Therefore, it is still not feasible, and experts say it will take years to obtain results. They started researching with the heart and researchers are also doing so with other organs: the liver, lungs, etc. This research is currently being carried out with mice. The theoretical basis is similar to the technique of Macchiarini, since an organ support of a donor and stem cells of the patient is needed. But the main difficulty lies in the need to create a whole solid organ.
Tailor-made organs: distant objective

For this purpose, a laboratory was opened at the Gregorio Marañón Hospital, directed by Dr. Francisco Fernández-Avilés. In Spain they are pioneers in this research. The same idea arose from Dr. Doris Taylor's research at the University of Minnesota and at Gregorio Marañón Hospital there is a follow-up to this work. Rafael Matesanza closely follows his work, with hope but caution. "It's very complicated. It will take time to achieve this, we will have to take previous steps, and when it is achieved in humans it will be the definitive moment. The day a heart of this type is transplanted to a patient there will be no turning back. And I think it will take a few years until we see it."
However, Matesanz does not believe that the techniques for the realization of these bioartificial organs can end the transplants we know today, "because we will always have the problem of urgent transplants."
Time will tell. At this time, the use of stem cells has aroused great hope, but we still have to wait long to see the results. "People always listen on television and in the press that stem cells perform miracles. That's nonsense, there's no certainty," says Macchiarin. But it is true that there is a great effort of research around them.
Dr. Matesanz is also prudent. "We have to have our legs on the ground," he says: "Stem cells have great potential, but they can remain in nothing. It has been 15 years since we started talking about stem cells, and we are still here. Precisely in the manufacturing technique of artificial organs it is necessary to see how much is advanced and what is achieved, but not in a single laboratory: it has to get well in one place, then in another, etc. And in the end it must be extended to all sites. That is the signal that is strengthening a technology."

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia