What is laryngectomy?
1990/04/01 Algaba, Jesus Iturria: Elhuyar aldizkaria

After reading this title you can think that many laryngectomized speakers speak. It is true, but talking to the air of the lungs or talking about the esophageal voice, that is, talking about the air previously ingested is not the same.
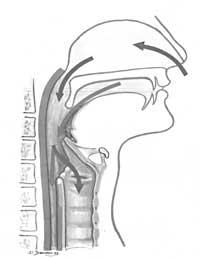
But how does the voice arise? In order for a person to speak he has to meet special conditions: hearing apparatus in good condition, appropriate neurosensory connections, air reservoir or lungs, phonator or larynx, appropriate nervous system and finally, echo area and cutting organs.
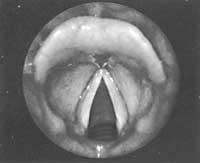
The larynx is a vibratory organ. Through the voice strings and other existing organs the air stream is modified and the voice is created. The voice changes in the pharynx, creating words.
What is a laryngectomized person?
Laryngectomized is a person who has had the larynx removed. Therefore, you have lost your natural voice and should breathe through the tracheostomy, that is, through the hole in front and under the neck after removing the larynx. But unfortunately, laryngectomized is something else. Through the larynx we can communicate verbally with people. It can be said that it is a mandatory organ for the discovery of our identity. Although some laryngectomized are called “esophageal voices”, others (approx. 50-60%) do not properly capture this type of voice.
In addition, when the patient is told that he has cancer and that a total laryngectomy must be performed, loss of voice is associated with a psychic depression. He usually becomes desolate and changes his way of being and in some cases commits suicide. The discomfort generated by the new situation makes the patient not assimilate correctly all the indications raised.
Sometimes it is necessary to insist on the indications about the disease and the anatomical and functional consequences that will suffer.
Here are some factors related to laryngectomy:
1.- Life
Fortunately, more and more patients are able to live. At this time the percentage of supervision ranges from 60 to 70%. Therefore, the next goal is to leave these people in the best situation for life, so that social, family and work life are as normal as possible.

2.- Lack of larynx
The removal of the larynx is the separation between the airway and the digestive tract. Therefore, the vibratory system of the vocal cords disappears and the air from the lungs is expelled from the tracheostomy. Consequently, this air cannot be used for fonation.
Swallowing will be normal after the postoperative period.
Removal of the larynx and glottic sphincter may cause discomfort in lifting, unjamming, or giving birth (in women) to heavy objects. The reason is that chest air cannot be fixed without closing the glottis.
3.- Tracheostoma
When the respiratory tract is separated from the digestive tract, the trachea is directed forward and the patient must breathe through it throughout his life.
The air, entering directly into the cowbell from the outside, is not heated, cleaned or moistened. As a result, the trachea is irritated and more mucus occurs causing coughing. Mucus can be dried and crusted. These can work as plugs obstructing the air.
The presence of tracheostomy forces the patient to take extreme precautions during the bath and shower.
4.- Effects by not passing air through the nose
Not passing air through the nose will cause loss of smell and decreased taste.
The mucus cannot be honestly done or expelled.
5.- Radiotherapy disorders
Stiffnesses, fibrosis and adhesions occur in the neck, changing the anatomy.
The irradiated tissues become edematized and hardened; the muscles can acquire lasting stiffness and the motor changes.
Another consequence of radiation therapy is the modification of salivary secretion, with strong dry mouth and pharynx at first.
6.- Psychological problems
Loss of voice is one of the most important factors in the appearance of psychological problems. According to different statistics, 50% of psychological problems are a direct consequence of loss of voice.
Having a bad disease and knowing whether or not it can be cured can cause depression and distress in the patient.
Feeling mutilated and having a hole in the neck can also cause psychological problems.

On other occasions, knowing that you will not be able to work normally and, therefore, will not be able to maintain the family properly, generates anguish.
7.- Family problems
Family problems will be conditioned by the patient himself, his family and his economic situation.
Changing personality and the psychological situation of the patient can make family relationships difficult. Family support will be of great importance in this problem. It is necessary to help the patient and it is the partners that most easily overcome these problems.
Sexual intercourse between spouses varies by 40%. Sometimes sexual activity increases, but in most cases it decreases. Sometimes it is due to the fatigue of the patient, but other times to the rejection of the couple who cannot stand tracheostomy.
8.- Social problems
These problems are closely related to the above problems. The sick fear facing life, the social environment or their friends.
The better the voice, the social problems are minor, as you can engage in a conversation between friends, for example.
9.- Labor problems
Most patients leave their jobs. Some change jobs and those who remain in the previous position are very few. Work problems have a lot to do with age, phoniatric situation, the situation of the patient, respiratory changes, economic problems, etc.
Possible for laryngectomized
The main task of doctors is to maintain life. Therefore, surgical, chemotherapeutic and radiotherapy treatments must be accompanied by a periodic control of patients, in order to detect whether the disease has been restored and provide a solution as quickly as possible.
Once life is assured, our goal is to provide a good quality of life. To do this, strengthening the relationships between the surgeon, the business doctor, social workers, the family and the worker himself can be very useful.
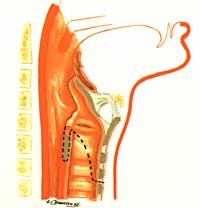
Theoretically the best thing is that the patient does not have tracheostomy, breathes in the natural way and has the voice as normal as possible. Therefore, we must approach these conditions, but without questioning the patient's safety at all.

Currently, in the line of recovering the voice, we can present three ways:
- Esophageal rehabilitation
- Electrolarynx
- Surgical rehabilitation
Historical summary of sampling voice recovery
a) At the same time as the total laryngectomy
Together with the total laryngectomy and for the patient to maintain the voice, surgical techniques of communication of the respiratory system with esophagus, pharynx or mouth will be addressed through a surgical procedure.
As soon as the total laryngectomies were started, the laryngologist knew that if the air from the lungs was passed into the pharynx or esophagus without the larynx, the voice obtained (even if it were a hive) was sufficient for communication.
In 1873, the first total laryngectomy of the BILLROTH hand was performed. One student, GUSSEMBAUER, was in charge of performing the prosthesis that linked the trachea and pharynx. In short, that's what we do today, a hundred years later.
In 1879 CASELLI and 1886 PARK connected one end of a metal prosthesis to a pharyngeal fistula and the other end to traceostoma. Through this path they achieved a good voice in two people.
In 1942 BRIANI performed a laryngectomy creating a pharyngostoma on the trachea. Then the prosthesis that linked the trachea and pharynx was placed and the patient spoke.
In 1958, CONLEY performed a tracheoesophageal fistula using a tube of mucosa from the trachea to the esophagus, which reached the top of the tracheostomy. In 1960, the ASAI joined the trachea and pharynx using a subcutaneous tube. All these techniques caused problems when swallowing and fistulas were clogged.
With the publication of the works of SERAFINI in 1970 an important step was taken in the recovery of the voice of the laryngectomized. Although the phonatory results were good, swallowing problems occurred and a large number of new cuts were required. Consequently, this technique was discarded.
In 1973 the STAFFIERI neoglotis phonatory technique was released and soon we began to apply all otolaryngologists. After total laryngectomy, it has been the most widely used in available voice recovery techniques. But here too the problem of swallowing is not solved correctly.
In 1978 AMATSU described its method for primary phonological fistuloplasty. He performed a fistula between the trachea and the esophagus, making a membranous pedicule with the back of the trachea.
In 1981 PANJE proposed a voice recovery method for laryngectomized people. At the same time the larynx is removed, a prosthesis will be placed between the trachea and the esophagus.
Also in 1981, I myself, together with my collaborators, began to make a personal change of technician AMATSU. Later we got what we wanted and we will inform you in another article of this technique.
In 1983 HERRMANN presented its glotoplasty technique, placing a prosthesis between the trachea and the hypopharynx.
In 1984 NIJDAN and its collaborators proposed placing the Groningen prosthesis at the same time as the total laryngectomy.
In 1985, HAMAKER, BLOM and SINGER proposed using their prostheses at the same time as total laryngectomy.
b) Voice recovery in people who are already laringectomized
Fistuloplasty
is more modern than the history of secondary phonatories. While in this field the beginning of the modern era was given by ASAI, there are others to mention.
In 1924, DELAVAN connected a patient's trachea and pharynx. Under the tongue, it makes a fistula outside the pharynx and connects it through a prosthesis to the tracheal stoma.
Four years later, SCURI operated fistula between the trachea and the pharynx of a patient, able to say words when covering the tracheostoma with the finger.
In 1931 GUTTMAN formed a tracheoesophageal fistula in a laryngectomized with a diatermic needle. This patient got a big voice covering the tracheostomy with her finger.
Between 1942 and 1959, BRIANI published several cases of voice recovery after total laryngectomy. Initially, the cutaneous tunnel went downward and backward joining the esophagus. He then made a change and developed the straight fistula, creating a pharyngostoma on the tracheostomy from the center line to the left. This pharyngostoma connects to the trachea through a complex prosthesis, obtaining a good voice and avoiding the entry of liquids and saliva to the trachea.
In 1960 ASAI began performing its third class of laryngoplasty in those who were already laryngectomized. This ASAI technique has pioneered the rest of the techniques.
In 1976, STAFFIERI unveiled the technique of its phonatory neoglotis. He also designed a prosthesis that was not only used in neoglotis defects. It was also used as deferred surgery in those who were already laryngectomized.
In 1979 SINGER and BLOM presented their tracheoesophageal puncture technique and their phonatory prosthesis. This cutting technique has undergone some changes and has been used by many laryngologists in their courts.
In 1981 I and my assistants started using a secondary technique in which they were already laryngectomized. This technique is similar to the primary technique called tracheal ascension.
In 1981 PANJE proposed another method of tracheoesophageal puncture. It can be performed under local anesthesia and in a traveling way. A rubber tube is inserted through the mouth and a point of the trachea is pressed.
We started using the SINGER-BLOM technique in 1981. Although initially we used general anesthesia, after some changes, we used local anesthesia.
In 1981 HERRMANN and KLEY presented their hypopharyngeal puncture method and prosthesis at the Hungarian World Congress.
A year later the GRONINGEN team presented the new tracheal puncture method and the new prosthesis. The prosthesis is inserted through the mouth and the tracheoesophageal wall is placed outside the interior. The prosthesis is also different from the previous ones.
In 1982 TRAISSAC presented a two-piece prosthesis. This prosthesis applies to STAFFIERI neoglotis defects and patients who have not achieved a good esophageal voice.
In recent years, many new techniques have been developed through technical changes in BLOM-SINGER, but basically similar.
The technical field of the disease will be discussed below.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia