Vaccines for tomorrow: DNA vaccines?
1998/09/01 Sarasua Etxeberria, Arantxa | Umaran Sanchez, Adelaida Iturria: Elhuyar aldizkaria
What are vaccines? It can be said that they are elements that drive a specific immune response. Vaccine molecules are called "antigens" and, although they are not pathogens, favor a specific defensive response as pathogenic microorganisms, but without causing disease.
The antigens of the first vaccines were live but attenuated or dead whole microorganisms. These vaccines have controlled smallpox, measles, or cough. Vaccines have been very effective and some of them are still used, although the antigens of each microorganism are not fully known. Live vaccines are more effective than months, but their main failure is insecurity. If there are errors in the buffer process or if used with immunodeficiency, the vaccine can cause disease.
Once the antigens that drive the protective response in the case of a specific disease are identified, antigenic protein vaccines can be made. To control meningitis, tetanus or diphtheria vaccines of this type have been used. As protein antigens have been purified, risks have been reduced, although their effectiveness has sometimes been lost. On the other hand, many microorganisms have developed the ability to hide or modify their antigens.
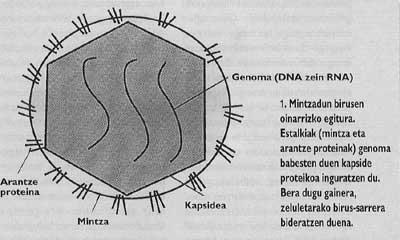
To overcome all these problems we have to look again for simplicity and for this we only have to go to the origin; identify, cut and directly introduce the genes that encode the antigens. This is how DNA vaccines were born. This DNA is in the form of plasmid, that is, it is a circular molecule that will not double in the cells of the vaccinated mammals, but will be synthesized and expressed strange proteins that encode.
All this has been achieved with vaccine-free infections and at the moment only the usefulness of these DNA vaccines has been shown with animals. The first figure shows the infectious diseases that kill children under 5 years of age. As you can see, many new vaccines are about to be made and these new DNA vaccines can serve to fill that gap.
Stimulate cellular immune response

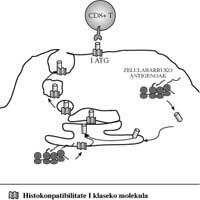
Virus infections are always intracellular infections; the parasite responsible for malaria and other protozoa live inside the cell. As long as they remain inside the host cells, antibodies cannot harm this type of parasite; antibodies can only block them by moving from one cell to another. Enhance cellular immune response for both detection and destruction of infected cells, such as activation of cytotoxic TD 8+ lymphocytes and macrophages, among others.
The DNA vaccine contains genes that encode several antigens from a microorganism, such as a virus layer protein. The host cell will internalize foreign DNA and form the virus protein in its cytoplasm. As if it were own proteins, in host cells class I molecules of complex dominant histocompatibility will carry the peptides of the viral protein to the cell membranes (Figure 2). These presentations will cause CD8+ T lymphocytes, so, unlike other vaccines, they will stimulate the cellular immune response 5.
On the contrary, protein vaccines, once inside cells through phagocytosis, will appear in membranes alongside class II molecules of complex dominant histocompatibility. This type of presentation will mainly ignite antibody response using CD4+ lymphocytes. In addition, with this endogenous pathway of antigen presentation, more epitopes are expressed than with other techniques, obtaining greater immunity 8.
Another feature of the response to DNA vaccines is the creation of a large number of type 1 auxiliary T lymphocytes. Macrophages will be activated and a very effective response will be achieved to eliminate surviving bacteria, such as Mycobacterium tuberculosis or Listeria monocytogenes within macrophages.
However, although the response to these vaccines is mostly cellular, exogenous DNA acts as a mitogen activating B cells and favoring antibody response 3.
Without vector
Another advantage of DNA vaccines is that no transport is needed, DNA is used naked as plasmid. Plasmids are circular DNA molecules capable of doubling spontaneously inside a bacterium, while in mammalian cells they will not double but contain the necessary elements to transcribe the genes they carry. Therefore, to cause an immune response, the gene we have chosen is inserted directly into the muscles by adding the plasmid, i.e. without using vectors. There it will be transcribed and then RNA will be returned in the ribosomes in the proteins.
All gene transfer systems demonstrated so far had to use vectors, that is, the selected gene entered the genome of a virus and the latter, the vector, was inserted into the host muscles. On the one hand, it is difficult to find an appropriate vector to transport any type of gene and on the other, subsequent damage by the vector is always dangerous.
Form as epitopes
Antigens used to promote immune response should maintain or imitate as faithfully as possible the three-dimensional shape of some parts of microorganism proteins. Otherwise, the antibodies generated by vaccines and T-cell receptors will not be sufficiently attached. Microorganisms, in the process of damping or inactivation, often alter the structure of proteins, with the consequent loss of antigenicity. In the case of DNA vaccines, the protein of the microorganism is formed within the cell and presents itself to the immune system without any change, so the integrity of the epitopes is maintained better and the response obtained will be more effective.
Ease of conjugation
As new vaccines are incorporated into the immunization schedule, the maintenance of vaccine use will become increasingly complicated. The solution would be to incorporate all the antigens at once, but if these are protein, especially if used in high doses, it is not possible to integrate them all at once.
DNA vaccines would allow, at least in theory, to apply the genes of different pathogenic microorganisms in a plasmid by juxtaposition. In any case, it will always be easier than conjugating the proteins encoded by each DNA.
Immunity is achieved against all mutant slags of a microorganism
Some viruses, to avoid our immune response, occasionally alter their surface antigens by creating new mutants or serotypes. Thus, despite the development of immunity against a serotype, when another mutant serotype appears our defenses are null. That is, what happens with the flu, since the vaccine is formed with protein antigens, serves for a single serotype and flu vaccination should be repeated annually.
Researchers have achieved a new DNA vaccine that protects animals against different serotypes by working with the influenza virus14. It seems that cytotoxic T lymphocytes that appear from this vaccine are associated with unmodified internal antigenic proteins. But to achieve this immunity these antigens must be presented endogenously. Other groups of researchers have obtained through DNA a vaccine against all papillomavirus serotypes and another vaccine against the herpes virus type II with animals 2.4.
Immunogens also in young children
To prevent infectious diseases we often have to protect young children and the response of this group is scarce. For the undeveloped immune system to provide sufficient response, it is necessary to use systems that strongly favor cellular response. To do this, DNA vaccines have a theoretical advantage.
On the other hand, in the case of measles, for example, antibodies taken from their mother steal the effect of live microorganism vaccines. The DNA vaccine will surely overcome this problem.
In addition, DNA vaccines, like other dead vaccines, will be safer from immunodeficiency than live vaccines. On the other hand, they will also be easier to use in many places in the world, since unlike proteins, they are thermoset.
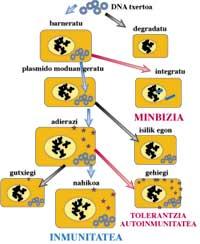
Cause cancer?
Is it capable of introducing external DNA into our chromosomes?
If so, DNA vaccines are over! The mutations that this would imply would alter all the processes of regulation of our cells and produce greater damage than we intend to prevent.
Cause tolerance or autoimmunity
Once the gene is introduced, and recognizing that it does not enter our chromosomes, how long will the gene encoded antigen be synthesized? If the host becomes tolerant to this antigen it can last a long time, so it would not respond in case of infection. The other possibility is to favor the phenomena of autoimmunity, considering that this antigen is being expressed in our cells along with the molecules of our complex and main histocompatibility, a group that favors the specific cytotoxic response. It would not be strange that in maintaining this situation for a long time there were damage by autoimmunity in the tissues of the host.
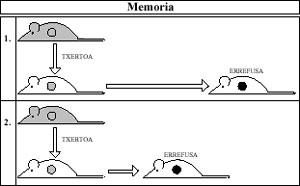
However, in cases tested so far, it seems that the expression period of foreign antigens is the most appropriate for the response to be effective and specific memory cells appear sufficient, but not sufficient to generate tolerance or autoimmunity 7 (Figure 3).
Overview for the creation of new vaccines
In the coming years this new technology of DNA vaccines will especially facilitate the formation of vaccines. Given the antigenic complexity of some microorganisms, this technology can be used in each case to identify the antigens that drive the protective response. It is also worth it if used exclusively for this, although other systems are then used to present these antigens to the immune system 9. The use of genotecs for the elaboration of DNA inserts and the choice of the most suitable antigens can be a general method for the realization of any type of vaccine. This technology has been used to select, among others, the most interesting antigens of the bacteria of the genus Mycoplasma 1.
Working on other ways to introduce DNA
Although DNA vaccines to date are for muscle integration, there is the possibility of creating DNA vaccines to be taken by mouth or mucous membranes. This option would be very interesting, for example, to prevent diarrhea. A team of researchers has already managed to use a cushioned Shigella slag to introduce DNA into the intestinal wall 11.
Vaccinating against cancer
So far we have talked about anti-infectious vaccines, but DNA vaccines in animals are being tested to control lymphomas 12. In the coming years DNA vaccines will also have interesting applications in the field of cancer.
Use a concrete and rigorous methodology to demonstrate safety
We now have the opportunity to assess the risks mentioned. To study the integration of DNA introduced into animal cells on chromosomes there is a specific methodology for the distribution of chromosomal and plasma DNA. Once the remaining plasma vaccine is excluded, chromosomal DNA should be analyzed to look for vaccine DNA using the PCR technique. This technique is very sensitive to detect a copy of the vaccine plasmid between 150,000 cells. In the case of influenza, the degradation of the plasmids incorporated by applying this methodology has been verified. (1.5.10 11 inserted copies and 6 weeks later 1.5.10 3 remain). On the other hand, in this case they have not found integrated copy in chromosomes 6.
Compare cost and benefit in each case
However, a case-by-case evaluation should be carried out and a comparison of the risks that may arise from the DNA vaccine with the possible damages arising from its non-use should be made. In the case of hepatitis B, for example, we should compare the probability of getting cancer from the vaccine with the decrease in the number of hepatocarcinomas we have achieved through vaccination 13.
Phases for the development of new vaccines
In any case, all the steps leading up to the market of a new vaccine must be successful: a) laboratory tests, for the formation of designed plasmids and for treating the vaccine with animals and b) clinical trials: in the first phase to demonstrate that the vaccine is not harmful with small groups of volunteers, in the second phase to choose the doses and vaccination guidelines with a large group and finally in phase 3, to show that the vaccinations are beneficial in figure 4. There are currently DNA vaccines that have been designed and tested with animals, but there are 15 clinical trials pending.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia