Diagnosis of pancreatic cancer
Nobody wants to hear anything about it and, if you have to listen to it, only in nightmares at night. If we are diagnosed with pancreatic cancer, our plans spoil and we extinguish our dreams.
Currently, pancreatic cancer is one of the most predicted neoplasms in the world. Although this type of cancer does not appear frequently, being the tenth most frequent tumor, its mortality is high and is the fourth most frequent cause of cancer death. It is estimated that only 5% of patients remain alive five years after cancer diagnosis.
Factors that cause poor prediction include delayed diagnosis of the disease and the nature of the tumor and response to current treatments.
Pancreatic cancer can be of several types, but the most common is ductal adenocarcinoma of the pancreas, which is 90% of all cancers.
This type of tumor comes from the exocrine cells of the pancreas, that is, from the cells that form the pancreatic juice and carry it to the intestine. Specifically, the latest findings indicate that the tumor is due to acinar cells. These cells first suffer cell differentiation and then differentiate into ductal cells. As a result, as these tumors end up having many ducats (vessels that carry pancreatic juice), they are called ductal adenocarcinomas of the pancreas.
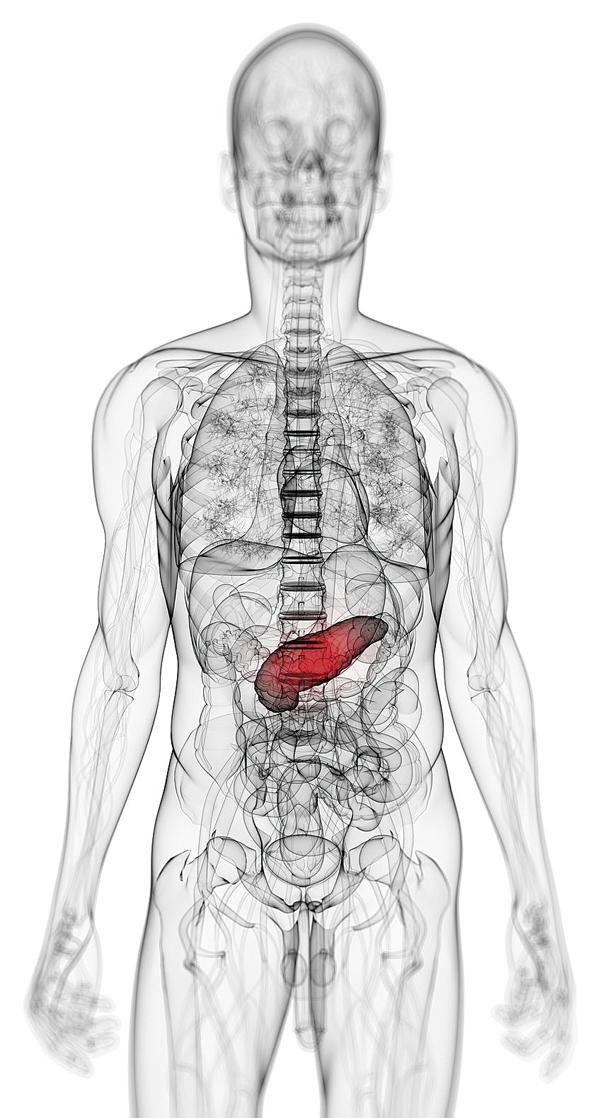
Approximately 60-70% of ductal adenocarcinomas of the pancreas are found in the head of the pancreas, 20-25% in the body or tail and the rest scattered throughout the organ. Although there are differences in the place of the pancreas where the tumor is located, the symptoms of patients are: weight loss, lack of appetite, abdominal pain, jaundice (yellow color in the mucous membranes, especially in the eyes, for having a high bilirubin), fatigue... These symptoms tell us that the person is sick, these symptoms remind us that pancreatic cancer is "silent".
Despite these symptoms, the diagnosis of this disease is a difficult task for gastroenterologists for various reasons. On the one hand, the pancreas is located anatomically behind the stomach and intestine, making it difficult to diagnose using imaging techniques. On the other hand, the symptoms of the disease are not very specific (sometimes pancreatitis and other types of tumors such as liver cancer have the same symptoms) and appear when the disease is advanced. Finally, there is no specific diagnostic marker for the disease. For all these reasons, pancreatic cancer is generally diagnosed when the disease is advanced and surgery is not always possible, and chemotherapy and radiation therapy are ineffective.
Only 15% of patients diagnose tumors when surgical removal is still possible. Currently, only surgery has shown that it is a real opportunity to cure the disease. Of this percentage of operable patients, 75% of them suffer a recurrence, approximately two years later.
That is... it is often late... its "silent" nature makes it diagnosed when the disease is advanced.
So the goal is to seek hope... to find ways to change what you feel when you know you have little time to fulfill your dreams. Find ways to communicate the news to keep dreaming and maybe even to make plans when there is time.
We need tools that allow us to diagnose the disease early so that patients can be intervened and respond to antitumor treatments.
Interestingly, recent studies indicate that the exocrine tumor of the pancreas takes at least ten years to develop, from an initial mutation of a cell until the patient is diagnosed with cancer. These data show that, apparently, we have a relatively wide margin (of a few years) to develop and improve tools that allow early diagnosis of the disease, thus improving the life expectancy of patients. We have time to achieve that one day after diagnosis we can continue to dream.
It seems evident, therefore, the need to investigate medical and scientific communities to facilitate an early diagnosis.
To this end, one of the most useful options is the search for molecular markers or biomarkers. These markers are biological molecules generated by the tumor and their detection (both in blood and feces) would allow us to specifically diagnose the disease in the early stage of development.
In this sense, and although in recent years there has been a basic and clinical research, the only marker in the clinic is glycoprotein CA19-9. It is sensitive and unspecific and there is a debate about its usefulness for diagnosis.
There is still a need to join forces in research to look for new markers, both in blood and stool or in pancreatic juice.
It must be recognized that the research and investment that has been carried out in this regard has been limited for several reasons: the difficulty of obtaining pancreatic tissue to carry out the research, which is often not operated on patients; the impossibility of conducting longitudinal investigations, since the life expectancy of patients is short; cultural and/or economic reasons make the investment unprofitable for governmental or pharmaceutical institutions.
Improving in this last aspect is still in our hands. Promoting and valuing research is the first step in prolonging patient dreams. Betting on research means having hope to make plans in the future, even after diagnosing pancreatic cancer.
Many biomedical centers around the world are conducting research to facilitate the diagnosis of pancreatic cancer and develop effective therapies for patients. New proteins, small RNA or methylation signals of genes that are now part of initial research may be the future of molecular diagnosis and personalized medicine of pancreatic cancer. New molecules that will allow us to continue dreaming.
Buletina
Bidali zure helbide elektronikoa eta jaso asteroko buletina zure sarrera-ontzian











